Chronic diseases such as diabetes, COPD, hypertension, and coronary heart disease are among the leading causes of death today. According to the latest CDC figures, 6 in 10 US adults have at least one chronic condition, while 4 in 10 have at least two or more.
As a major cause of death and disability among various patient populations, chronic diseases account for a significant chunk of the $4.1 trillion annual healthcare costs in the US. Tobacco use, poor diet, and an inactive lifestyle contribute to the increasing incidence of chronic diseases.
Providing adequate care for the chronically ill is a major challenge as it requires coordination between primary care physicians, specialists, and physical therapists. Continuous patient care, periodic doctor visits and appointments, long-term medications, and therapies are often necessary to manage the condition.
It was in this backdrop that the Centers for Medicare and Medicaid Services (CMS) introduced Chronic Care Management (CCM) in 2015. The main goal of this initiative is to improve the quality and coordination of healthcare services available to Medicare patients with multiple chronic diseases.
Medicare defines chronic care management as ‘non-face-to-face visits provided to patients who have multiple significant chronic conditions expected to last at least 12 months.’ More than a third of the US population would fall under this definition.
Given the sheer scale of the problem, CCM should be a top priority for all healthcare providers in the US. To efficiently handle the CCM needs of patients, you need chronic care management systems.
Frequently Asked Questions About Chronic Care Management Services

Why Should a Healthcare Practice Have a CCM Program?
There are three major reasons why a CCM program can be a game-changer for a healthcare practice. These include:
Improved Patient Health
The most important reason to add a CCM program to any medical practice is to improve clinical outcomes for patients with chronic diseases. Regular calls between the patient and a qualified care provider will ensure that there is consistency in the treatment and management of chronic diseases.
Using telehealth technology, such calls fill the gaps between routine checkups and visits to the doctor’s office. Patients of healthcare practices with a chronic care management program tend to have a better quality of life and improved long-term outcomes.
Reduced Staff Workloads
Another critical aspect is decreased workload on administrative staff. These days, more than 80% of the communications between a patient and their healthcare provider happen over phone calls. Even a small family practice can expect up to 1600 calls from patients in a single week.
For smaller administrative teams, the sheer volume of these incoming calls can present a formidable burden. When you partner with a CCM provider that has the capacity to handle care delivery, it will free up a lot of time for the office staff.
Increased Revenue Streams
Patient phone calls are usually non-billable and can take up a lot of precious time at a doctor’s office. With trained care coordinators handling such calls, the clinic/practice can focus on more productive tasks, handling patients who are physically present at the premises.
Another highly lucrative factor is Medicare reimbursements. They are contingent on the practice hitting certain thresholds in terms of the number of patients enrolled in CCM. Some providers earn up to $100,000 in additional revenues from Medicare reimbursements.
Based on this, the documentation required to make that happen can be quite considerable, taking up a lot of administrative time. Having a CCM program like HealthSnap can provide a tangible boost here, improving patient health and safety, and more importantly, reducing the workload on office staff.
How to Successfully Implement a CCM Program?
Successful implementation of a CCM program hinges on the creation of proper operational groundwork. There are several sequential steps to be taken care of, including the following:
1. Plan and Create a Chronic Care Team
Creating an in-house team for CCM can be quite challenging. You will need considerable technical and technological resources, as well as skilled care managers who should either be registered nurses, nurse practitioners, certified medical assistants, or health coaches.
Assembling them all under a single roof is not easy. Co-sourcing the CCM program to a proven third-party service provider like HealthSnap is a far more practical and logical solution. By partnering with an established CCM vendor you will provide your patients with a concierge level of care between office visits, without disrupting existing office workflows.
If the practice already has existing EHR software, it will have to be integrated into the IT software and systems of the CCM program. A better alternative would be to find a provider that offers an integrated software solution that combines both EHR and CCM into a single package.
HealthSnap online platform contains integrations for 80+ EHR solutions in the market. With HealthSnap’s team and technology on your side, you don’t have to worry about having to handle two separate IT solutions for patient data management.
2. Shortlist Eligible Patients for the Program
Once you have the chronic care team and the CCM program assembled and ready to go, it is time to add eligible patients to the program. The eligibility criteria laid out by Medicare is quite clear and unambiguous.
You can use your existing EHR databases to identify patients with at least two chronic diseases who have consulted your practice in the last 12 months. Ideally, you will need an EHR with an integrated CCM solution.
A chronic care management software solution is designed and built to manage Medicare programs, something that is not part of the primary functions of EHR software.
Once you have a list of potential candidates, you can identify the patients who are best suited for chronic care management, based on common conditions like diabetes and COPD. Given the 80% coverage from Medicare for Part B populations, you may also want to target your Medicare B populations at this point.
3. Recruit Shortlisted Patients to the CCM Program
The best way to recruit a patient is by introducing the program to them during a checkup or routine visit to your practice. When a doctor explains the benefits in-person, the patient is more likely to enroll.
Other potential options to gain patient consent include phone calls, emails, or letters detailing the benefits of the CCM program to eligible patients. Once a patient agrees to participate, they will have to provide written or verbal consent.
This is best done by inviting the patient for a visit to the practitioner’s office or by initiating a telehealth visit. Both visit types (remote or in-person) ensure you are compliant and enrolling already established patients into your CCM program.
The visit also gives you a chance to check the insurance coverage of the patient. Medicare will cover 80% of the costs – if the patient does not have any additional third-party coverage, they will have to pay the balance of 20% as a copay.
4. Deliver Chronic Care Management Services to Patients
A practical way to introduce CCM to a patient is by scheduling annual wellness visits. After that, you will have to create a comprehensive patient-centered treatment/maintenance plan that addresses their myriad healthcare needs.
Share copies of the plan with the patient and your care provider teams. The plan will act as the guideline for all future care provided to the patient as part of chronic care management.
5. Submit Claims to Medicare CMS
To successfully receive reimbursement from Medicare for your chronic care management program, you will need to submit comprehensive documentation including specific CPT codes, ICD 10 codes, accurate details of all dates and places of service, and an NPI number.
The claims have to be submitted on a monthly basis to the CMS, and a corresponding invoice should also be sent to all patients concerned. Sending accurate data without any conflicting codes can be a tough ask without capable care coordination software.
What are the Benefits of Co-Sourcing a Chronic Care Management Program?
There are three important benefits to your practice from co-sourcing a CCM program to a third-party service provider:
Access to Experience
Implementing a chronic care management program that fits the exacting requirements set by the CMS (Medicare) is no easy task. To complicate matters further, all the terms related to enrollment, billing, and delivery could change every year. With a seasoned and committed CCM provider, you get access to experts who specialize in compliance and best practices.
Less Workload
The best CCM partners bring clinical care management services, IT resources & seamless integrations into your existing Electronic Health Record (EHR), and a comprehensive array of CMS-compliant care plans to your organization. These resources are flexible and can be tailor-made to suit your practice’s unique needs. They also come with the promise of scalable growth. With all this, you can significantly reduce the formidable workload needed to get a chronic care management program off the ground and sustainable at scale.
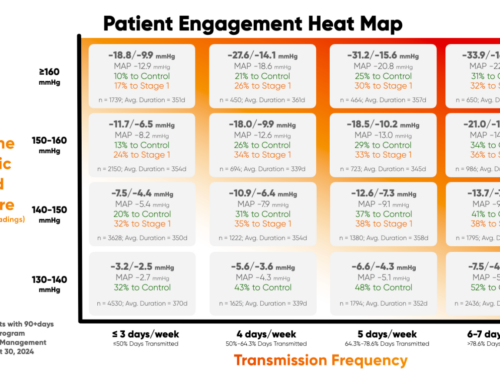
Improved Patient Engagement
The success of a chronic care management program relies heavily on patient engagement. Through consistent and relentless communications, the CCM teams can drive patient participation in your treatment plans. This way, you can improve not just patient improvement and satisfaction without your service, but also clinical outcomes.
What Types of Services are Provided Under CCM?
Many different patient services are included in a chronic care management service. Chronic care management includes:
- Creating measurable treatment goals
- Calibrating expected outcomes and general prognosis
- Medical management and symptoms management
- Caregiver assessments and planned interventions
- Coordination with outside practitioners and specialists
Can CCM be Provided in Other Settings Outside a Doctor’s Office?
Yes, a provider’s office is just one of the several settings where chronic care management can be provided under general supervision. Other common settings include community spaces, care homes, assisted living spaces, and in-home settings. Apart from in-person communication, CCM can be provided via telephone and online communications.
Do Telehealth Rules Apply to Chronic Care Management?
Telehealth is governed by a complex and stringent set of regulations, spread across both federal and state levels. While CCM does make use of telephone and online communications, telehealth regulations do not apply here.
Can CCM Services Be Completely Delegated to Clinical Staff?
Billing practitioners are expected to retain a tangible level of involvement in the chronic care management of their enlisted patients. They cannot delegate this duty completely to other individuals or entities.
For instance, CCM Service Codes are designed in such a way that compliance requires the medical practitioner to handle certain aspects of ongoing work. This can include general oversight, patient management, collaboration with other physicians, and reassessment of the patient’s health status to appropriately adjust the care plan.
Further, major medical decision-making, (governed by CPT codes 99487, 99489), are activities that cannot in any form be delegated to others by the billing practitioner. Reporting services is another activity (CPT codes 99491, 99437) that has to be handled directly by the billing practitioner. They have to come directly from the practitioner themselves.
Can the Clinical Staff Aspect of CCM Be Handled by Third-Party Companies Through Co-Sourcing?
Oversight at all times is the key deciding factor here – if the billing practitioner retains functional oversight at levels that are considered in compliance with the established “incident-to” and “general supervision” rules and regulations, clinical staff duties can be co-sourced to qualified third-party vendors.
Are the Billing Practitioners Required To See Their CCM Patients Face to Face?
Yes, an initial preventive physical exam (IPPE) is essential when a new patient who has not seen a doctor in the last 12 months is inducted into the CCM program. Further, billing practitioners are expected to encourage annual wellness visits when adding a new patient to the program. Based on these rules, a billing practitioner will have to see a CCM patient at least once in the last 12 months either face-to-face or through a telehealth visit prior to enrolling them in a CCM program.
Can More Than One Clinical Team Member Provide CCM Services During a Calendar Year?
There are no specific restrictions in the CCM regulations regarding this. As long as your practice meets all the regulatory requirements, the CCM services can be provided by more than one clinical team member in certain situations.
Example 1: if the original person responsible for providing CCM is on leave or resigns, or takes over other duties, another clinical team member can step in.
Example 2: as long as they operate within their scope of practice, team members can contribute to the delivery of CCM services in a specific month.
Does the Patient Have to Provide Consent in Writing for Access to CCM Services?
At the time of induction into the CMS program, the billing practitioner can receive explicit consent from the patient either in written or verbal form. If it’s verbal consent, the health record should document the date and time at which the consent was received in the patient’s chart.
Are Electronic Healthcare Technology Systems Mandatory to Document CCM Services?
Yes, the billing practitioner/healthcare provider should maintain a certified electronic health record (EHR) of each CCM patient. The treatment plans devised for each patient must be shared with all chronic care team members. The plan can be shared by digital means or fax.
Only the healthcare provider is required to use an EHR system. The community-based organizations (CBOs) that provide CCM services under the supervision of a healthcare specialist are not required to use EHR.
Will Medigap Cover the Beneficiary Cost-Sharing for CCM Services?
Yes, Medigap insurers cannot deny copay, coinsurance, or other benefits payable on behalf of the beneficiary under contract if the services are covered under Medicare Part B. The only exception would be if the Medigap policy has a deductible that is not met by the situation. In all other instances, private insurance plans must accept a notice of Medicare payment as a claim for Medigap benefits.
Can CCM Services be Provided by Physicians, Registered Clinical Nurse Specialists, Non-Physician Practitioners, or Other Staff Located Outside the US?
No, non-emergency Medicare services provided by individuals located outside the United States cannot be billed under current regulations. The same rule also holds if the beneficiaries are located outside the country. All involved parties should be present inside the United States.
How Can Non-Physician Practitioners Participate in the Delivery of CCM Services if They Cannot Bill these Services Directly?
Certified Medical Assistants (CMAs), Licensed Professional Nurses (LPNs/LVNs), and registered nurses (RNs) are examples of non-physician practitioners (NPPs) who cannot bill directly for CCM services delivered. Under current CMS guidelines, these NPPs can participate in chronic care management as clinical staff under the supervision of qualified NPPs or health care providers.
As members of a chronic care team, NPPs can perform a wide range of CCM services, including structured data collection, care management, providing access to chronic care, and other support services to facilitate CCM.
Who Qualifies As “Clinical Staff” Under CMS Guidelines and CCM Codes?
The CPT has an established definition of the term “clinical staff” for billing practitioners. Other major rules to consider are provided at 42 CFR 410,26 – which provides “incident to” rules for the proper definition of valid clinical staff under the Medicare CMS program.
You can only bill the time spent by clinical staff who qualify under the rules mentioned above. While other auxiliary staff can provide or facilitate CCM services to patients, they cannot be billed under CMS guidelines.
HealthSnap – Driving Proactive Patient Care with Every Interaction
HealthSnap is a leading Virtual Care Management solution that provides highly scalable Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) services to healthcare providers and health systems. We provide integrations with over 80 EHR solutions on our virtual care platform – you don’t have to work with two IT systems for patient management.
Other standout features include patented tools to predict and generate reimbursement reports for RPM & CCM, cellular-enabled patient health monitoring devices, and tools that give a holistic view of your patient’s health in one place.
If you are a qualified health-care professional considering RPM and/or CCM services for patients with multiple chronic conditions, HealthSnap is the platform for you. To learn more about HealthSnap and our Virtual Care Management platform, schedule a free demo today. Call us at 888-780-1872, or use the scheduling options on this page.