In 2018, CMS began providing standalone reimbursement for Remote Patient Monitoring (RPM) services. The final 2019 Medicare Physician Fee Schedule (“2019 MPFS”), released on November 1, 2018, created several new RPM codes for 2019 in the category of Chronic Care Remote Physiologic Monitoring, now referred to as “Remote Physiologic Monitoring Treatment Management Services” (“RPM”). These codes became effective as of January 1, 2019 and may provide reimbursement opportunities for HealthSnap’s customers. Importantly, despite the initial named reference to these codes as “Chronic Care” Remote Physiologic Monitoring, CMS has confirmed that use of these codes is NOT limited to patients with chronic conditions.
The final 2020 Medicare Physician Fee Schedule (“2020 MPFS”) added yet another code to the RPM to provide reimbursement for each additional 20 minutes of time spent providing RPM monitoring services. The 2021 Medicare Physician Fee Schedule (“2021 MPFS”) provided additional updates to the rules for reimbursement associated with these codes.
What are the Remote Patient Monitoring (RPM) CPT Codes?

CPT Code 99091
The 2022 CPT Code Manual describes 99091 as the following:
CPT code 99091 ($56*) – Remote Patient Monitoring (RPM)
Collection and interpretation of physiologic data (e.g., ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient and/or caregiver to the physician or other qualified health care professional, qualified by education, training, licensure/regulation (when applicable) requiring a minimum of 30 minutes of time.
Key Requirements for Billing CPT Code 99091
- Initiation of RPM services via face-to-face visit for patients not seen by the billing practitioner within 1 year prior to billing CPT code 99091; Waived for COVID-19 PHE.
- Patient consent must be documented in the patient’s medical record. As of January 1, 2021, this can be obtained at the time of the service;
- At least 30 minutes of time spent by the billing practitioner during a 30-day period reviewing, interpreting, and responding to RPM data; and.
- Review, interpretation, and response to data must be conducted by the billing practitioner (a physician or qualified healthcare professional (“QHCP”)).
Remote Physiologic Monitoring Codes
The 2019 MPFS described each of the original RPM codes as follows:
CPT code 99453 ($19*)
Remote monitoring of physiologic parameter(s) (e.g., weight, blood pressure, pulse oximetry, respiratory flow rate), initial; set-up and patient education on use of equipment.
CPT code 99454 ($55*)
Remote monitoring of physiologic parameter(s) (e.g., weight, blood pressure, pulse oximetry, respiratory flow rate), initial; device(s) supply with daily recording(s) or programmed alert(s) transmission, each 30 days.
CPT code 99457 ($50*)
Remote physiologic monitoring treatment management services, clinical staff clinical staff/physician/other qualified healthcare professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; first 20 minutes.
CPT code 99458 ($40*)
Remote physiologic monitoring treatment management services, clinical staff clinical staff/physician/other qualified healthcare professional time in a calendar month requiring interactive communication with the patient/caregiver during the month; each additional 20 minutes.
*Please Note: Reimbursement amounts listed represent a national average; exact reimbursement amounts vary by geographic region. Amounts are based on CMS 2022 non-facility pay rate and are subject to change.
Key Requirements for Billing CPT Codes 99453, 99454, 99457, & 99458

According to the 2019 MPFS and the 2022 CPT Code Manual, CMS requires the following to bill for Remote Patient Monitoring services:
General
- Medical Device. Devices used for RPM services must meet the definition of a “medical device” as defined by the U.S. Food and Drug Administration (“FDA”) in the Food, Drug & Cosmetics Act (“FD&C Act”). The FDA defines “medical device” as “an instrument, apparatus, implement, machine, contrivance, implant, in vitro reagent, or other similar or related article, including a component part, or accessory which is . . . intended for use in the diagnosis of disease or other conditions, or in the cure, mitigation, treatment, or prevention of disease . . .”. This does NOT mean that a device used must necessarily go through the FDA “clearance” or “approval” process for reimbursement purposes, but the FDA may require this depending on the device’s status under applicable FDA pathways. This means that the device would either need to be subject to current FDA “enforcement discretion”, registered, cleared via 510(k) submission, or approved via a Premarket Approval (“PMA”) application. Importantly, the FDA’s definition of a “medical device” also includes certain software functions. Further, according to the 2021 MPFS, the device must be “reliable and valid”, and the data collected must be automatically transmitted rather than self-reported.
- Billing Practitioner. RPM services must initially be ordered by a physician or other QHCP. In all cases, practitioners must practice in accordance with applicable state law and scope of practice laws.
- No Chronic Conditions Limitation. As stated above, although CPT codes 99453-99458 were initially described in the MPFS and CPT Code Manual as “Chronic Care Remote Physiologic Monitoring Services,” this language has since been adjusted to clarify that these services are not limited to patients suffering from chronic conditions. CMS finalized in 2020 that RPM services can be delivered to patients with acute conditions and beginning with the 2021 CPT Code Manual now describes these codes as “Remote Physiologic Monitoring Treatment Management Services.”
CPT Codes 99457 & 99458
- Initiation of RPM Services via Face-to-Face Visit
- For new patients or patients not seen by the billing practitioner within one year prior to billing CPT code 99457, CMS has indicated – but not actually required in the MPFS – that the RPM services should be initiated during a face-to-face visit with the billing practitioner. This face-to-face visit should be billed separately and may be an Annual Wellness Visit, an Initial Preventive Physical Exam, Levels 2-5 Evaluation and Management (“E/M”) visit, or the face-to-face visit included in TCM services (CPT codes 99495 and 99496).
- In response to the PHE, CMS finalized on an interim basis that RPM services can be furnished to new patients as well as to established patients. Therefore, for the duration of the PHE, RPM services can be provided to a new patient without an initiating visit. Upon expiration of the PHE, Medicare will again require that RPM be furnished only to established patients. There is some uncertainty regarding whether Medicare will allow a “face-to-face initiating visit” to take place via telehealth post-PHE, or whether Medicare will re-institute its requirement that a telehealth visit may be reimbursed only after a patient relationship has been established in person.
- Live, Interactive Communication. CPT codes 99457 and 99458 both require at least one interactive communication with the patient or caregiver during the calendar month. In the 2021 MPFS, CMS clarified that “interactive communication” refers to “at a minimum, a real-time synchronous, two-way audio interaction that is capable of being enhanced with video or other kinds of data transmission.”
- No duplicative concurrent billing
- CPT codes 99457 and 99458 can be billed in conjunction with the following:
- CCM codes 99487, 99489, 99490, 99491, 99437, and 99439;
- PCM codes 99424, 99425, 99426, and 99427;
- TCM codes 99495 and 99496; and
- Behavioral health integration (“BHI”) services codes 99484, 99492, 99493, and 99494.
- However, the billing practitioner cannot count the same period of time for more than one code, and no time can be counted on a day when the billing practitioner reports an E/M service for the same beneficiary.
- RPM and RTM CPT codes should not be billed for the same patient in the same month. The 2022 CPT Manual states that 98980 should not be reported in conjunction with 99457.
- The CPT Code Manual states that CPT code 99457 cannot be reported in the same calendar month as CPT code 99091, but CMS stated in the 2021 MPFS that there may be instances where doing so is appropriate. Providers should use their best judgment in determining whether it is appropriate to bill CPT codes 99457 and 99091 in the same calendar month.
- CPT codes 99457 and 99458 can be billed in conjunction with the following:
CPT Codes 99453 & 99454

CPT code 99453
- Use this code to report setup and patient education on the use of the device(s) that will be used to monitor their physiologic data. Services provided under this code can be furnished by auxiliary personnel (including non-clinical staff), which may include both contracted and employed individuals. This allows for RPM vendors to deliver this service on an outsourced basis to further ease the burden on their provider customers.
- CPT code 99453 may only be reported once per episode of care. For purposes of RPM, an “episode of care” begins when the service is initiated and ends when targeted treatment goals are attained.
- CPT code 99454
- Use this code to report supply of a connected device or devices for daily recording or programmed alert transmissions.
- CPT code 99454 can be billed once during each 30-day period.
- CPT codes 99453 and 99454
- Do not report either code when the time spent providing the respective services is included in the time spent for other RPM codes (e.g. 99457).
- CPT codes 99453 and 99454 may only be billed when there are at least 16 separate days of readings transmitted to the provider in the relevant 30-day period.
- Both codes can be reported in conjunction with devices that will be used for CPT codes 99457, 99458, or 99091.
- Due to the possibility that many patients with COVID-19 may not need to be monitored for as many as 16 days, CMS has currently reduced this requirement to require only 2 or more days of monitoring only for patients with a suspected or confirmed case of COVID-19.
Remote Patient Monitoring (RPM) Billing Considerations

Incident-To Billing of Clinical Staff Under CPT Codes 99457 and 99458
A clinical staff member is defined in the CPT Manual as “a person who works under the supervision of a physician or other qualified health care professional and who is allowed by law, regulation, and facility policy to perform or assist in the performance of a specified professional service, but who does not individually report that service.” This means that the type of personnel that qualify as “clinical staff” for purposes of RPM varies by state law and providers should look to the applicable scope of practice laws in the patient’s state to determine who can and cannot provide monitoring services.
CPT codes 99457 and 99458 allow for clinical staff members to provide RPM services under the billing practitioner’s supervision. When a billing practitioner reports clinical staff time, the billing practitioner bills contributing clinical staff members’ time on an “incident-to” basis. In general, services provided on an incident-to basis must be performed under direct supervision of the billing practitioner, meaning the billing practitioner must be in the same physical office location as the clinical staff. However CPT codes 99453, 99454, 99457, and 99458, which CMS designated as care management services, allows for the clinical staff member(s) or auxiliary personnel, as applicable, to be supervised under general supervision, meaning the billing practitioner must be available to answer a question or provide assistance, but does not necessarily have to be located within the same office building.
Care Management Services Under General Supervision
More broadly speaking, all care management services, including RPM, CCM, PCM, TCM, BHI, and psychiatric collaborative care model (“CoCM”) services, may be provided under general supervision by outsourced clinical staff. Per 42 CFR § 410.26(b)(5), “[d]esignated care management services can be furnished under general supervision of the physician (or other practitioner) when these services or supplies are provided incident to the services of a physician (or other practitioner).” In the 2020 MPFS, CMS referenced this regulation, stating that “[t]he physician (or other practitioner) supervising the auxiliary personnel need not be the same physician (or other practitioner) who is treating the patient more broadly.”
Further, CMS clarified in an FAQ that “[a] billing physician (or other appropriate practitioner) may arrange to have CCM services provided by clinical staff external to the practice (for example, in a case management company) if all of the “incident to” and other rules for billing CCM to the PFS are met.” Because the other care management services follow the same billing requirements as CCM, CMS’ clarification applies to all care management services provided under general supervision. This allows for a fully outsourced model in which one company provides RPM services (or other care management services as outlined above) for a particular patient population via clinical staff and/or auxiliary personnel (similar to the model commonly used for CCM services).
MACRA’s Quality Payment Program and RPM Services
Physicians and other eligible practitioners participating in the Merit-Based Incentive Payment System (“MIPS”) track of the Quality Payment Program under the Medicare Access and CHIP Reauthorization Act may benefit from providing RPM services for their patients. Under MIPS, the clinical practice improvement activity called “Engage Patients and Families to Guide Improvement in the System of Care” is now classified as a “high-weighted” activity – thereby incentivizing the use of RPM technologies (including RPM) that provide real-time feedback to patients and their care team. Another clinical practice improvement activity called “Use of CEHRT to Capture Patient Reported Outcomes” remains from Year 1 as a “medium-weighted” activity and involves use of digital tools to capture health data from patients.
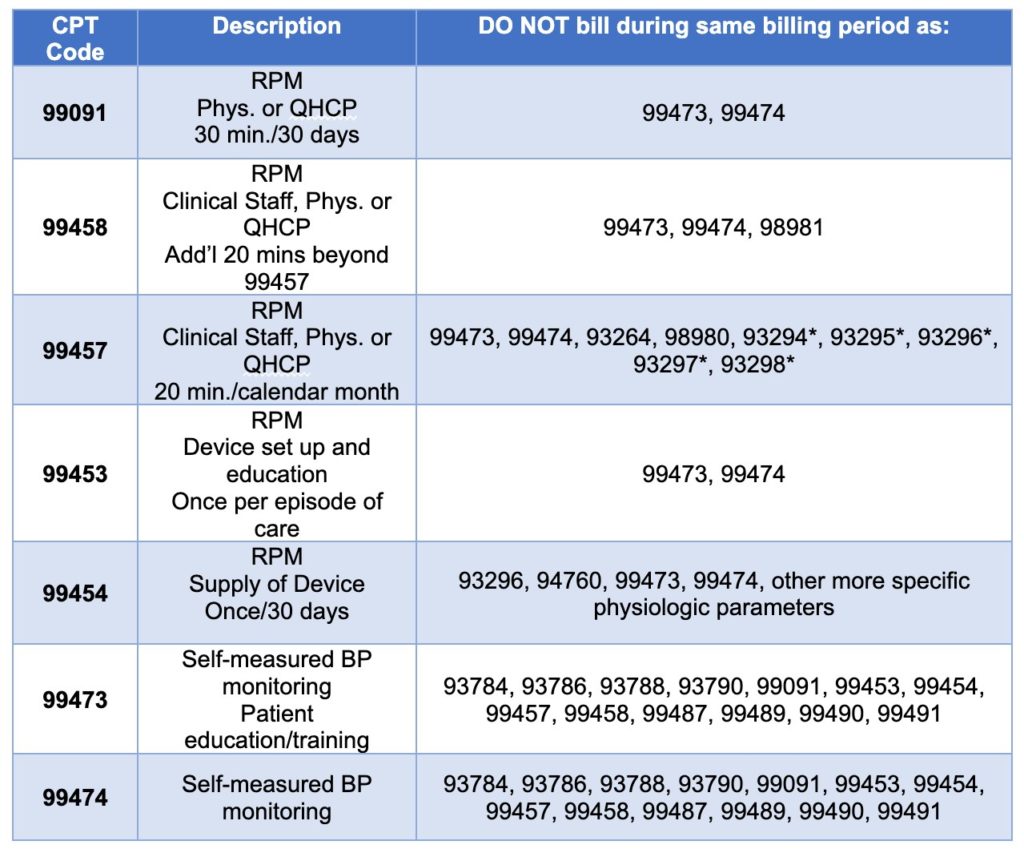
Remote Patient Monitoring Billing Restrictions
Start and Scale an RPM Program to Make The Most of RPM CPT Codes With HealthSnap
The COVID-19 pandemic forever changed the way that healthcare is delivered. Now more than ever, we’re seeing a rise in care delivered when and where patients need it most: in the home. By using the HealthSnap RPM program featuring cellularly connected RPM devices and an interface that directly integrates with over 80+ EHR systems, you can not only improve the health outcomes of patients with chronic conditions and use patient real-time patient data to make informed clinical decisions, but improve your bottom line as well.
Are you a provider interested in leveraging RPM CPT codes in your practice, FQHC, ACO, or health system? Book a demo with the HealthSnap team today to get started!






