Principal Care Management (“PCM”) refers to the practice of providing care to patients with a single chronic condition. To qualify for PCM, the patient must have a single complex chronic care diagnosis expected to last between three months and a year, or until the death of the patient, that may have contributed to a recent hospitalization, or that places a patient at significant risk of death, acute exacerbation/decompensation, or functional decline. PCM services also require the development, monitoring, or revision of disease-specific care plan; and ongoing communication and care coordination between providers who are involved in a patient’s care. In the 2022 MPFS, CMS added four PCM codes to further recognize that providers, who furnish services to patients with complex conditions, require more resources.
What are the Principal Care Management (PCM) CPT Codes?
The PCM codes are described as follows:
CPT Code 99424 ($83*)
Principal care management services, for a single high-risk disease, with the following required elements:
- One complex chronic condition expected to last at least 3 months, and that places the patient at significant risk of hospitalization, acute exacerbation/decompensation, functional decline, or death,
- The condition requires development, monitoring, or revision of disease-specific care plan,
- The condition requires frequent adjustments in the medication regimen and/or the management of the condition is unusually complex due to comorbidities,
- Ongoing communication and care coordination between relevant practitioners furnishing care;
- First 30 minutes provided personally by a physician or other qualified health care professional, per calendar month.
CPT Code 99425 (add-on code to 99424) ($60*)
Each additional 30 minutes provided personally by a physician or other qualified health care professional, per calendar month
CPT Code 99426 ($63*)
Principal care management services, for a single high-risk disease, with the following required elements:
- One complex chronic condition expected to last at least 3 months, and that places the patient at significant risk of hospitalization, acute exacerbation/decompensation, functional decline, or death,
- The condition requires development, monitoring, or revision of disease-specific care plan,
- The condition requires frequent adjustments in the medication regimen and/or the management of the condition is unusually complex due to comorbidities,
- Ongoing communication and care coordination between relevant practitioners furnishing care;
- First 30 minutes of clinical staff time directed by physician or other qualified health care professional, per calendar month.
CPT Code 99427 (add on code to 99426) ($48*)
Each additional 30 minutes of clinical staff time directed by a physician or other qualified health care professional, per calendar month
*Please Note: Reimbursement amounts listed represent a national average; exact reimbursement amounts vary by geographic region. Amounts are based on CMS 2022 non-facility pay rate and are subject to change.
Key Requirements for Billing the Principal Care Management (PCM) CPT Codes
The 2020 MPFS sets forth several important requirements that must be met in order to bill the PCM codes for services provided to a particular patient. Those requirements are as follows:
- Billing Practitioner. The billing practitioner for PCM services must be a physician or other QHCP. Though it is not an explicit requirement, CMS states in the 2020 MPFS that they expect most PCM services will be provided and billed by specialists focused on managing patients with a particular complex chronic condition that requires substantial care management. According to the 2020 MPFS, the expected outcome of the provision of PCM services is for the patient’s condition to be stabilized by the treating specialist clinician so that overall care can be returned to the patient’s primary care practitioner.
- One Complex Chronic Condition. The 2022 MPFS states that a single high-risk complex chronic condition:
- Will be expected to last between 3 months and 1 year, or until the death of the patient;
- Places a patient at significant risk of hospitalization, death, acute exacerbation/decompensation, and/or functional decline; and
- Requires frequent adjustments in the medication regimen and/or the management of the condition is unusually complex due to comorbidities; and
- Requires development, monitoring, or revision of disease-specific care plan; and
- Requires ongoing communication and care coordination between relevant practitioners furnishing care.
- Not Limited to 1 Condition. The 2020 MPFS implies that it is possible for a patient to receive PCM services from multiple specialists for multiple different conditions simultaneously (e.g. a cardiologist for arrhythmia and an endocrinologist for diabetes); however PCM services should not be furnished or billed at the same time as:
- Other care management services by the same practitioner for the same beneficiary; or
- Interprofessional consultations for the same condition by the same practitioner for the same patient.
- Ongoing Communication. Ongoing communication and care coordination between all practitioners furnishing care to the beneficiary by the billing practitioner in the patient’s medical record.
- General Supervision. CPT codes 99426 and 99427 allow for PCM services to be provided by clinical staff incident-to the billing physician or QHCP. These services can be provided under general supervision, meaning the billing practitioner need not be co-located in the same office as the clinical staff member providing the services, but must be available to the clinical staff member to answer questions and intervene when necessary. NOTE: CPT codes 99424 and 99425 are limited to services personally performed by a physician or other QHCP. Therefore, services provided by clinical staff cannot be billed for under CPT codes 99424 and 99425.
- Initiating Visit. For new patients and patients not seen within a year prior to initiation of PCM, the billing practitioner must conduct an initiating visit with the patient in order to educate the patient on PCM and obtain the patient’s informed consent. This visit can be an Annual Wellness Visit or other separately billable visit.
- Consent. The billing practitioner must obtain the patient’s informed consent and document that consent in the patient’s medical record. Consent can be obtained verbally, but the patient should be educated as to:
- What PCM services are;
- That only 1 practitioner can bill per month for an indicated chronic condition;
- The fact that the patient has the right to stop the services at the end of any service period; and
- Any cost-sharing that may apply.
- Concurrent Billing with RPM. PCM services can be billed in the same month or billing period as RPM services, so long as the time spent providing services under each is not counted twice. In other words, the time requirements set forth under each applicable code must be met separately in order for the services to be billable.
- Disease-Specific Care Plan. Under CCM, practitioners are required to develop a comprehensive care plan in order to bill relevant CCM codes. For PCM, CMS set forth in the 2020 MPFS that billing practitioners should instead develop a disease-specific care plan for patients receiving PCM services. A disease-specific care plan is more limited than a comprehensive care plan, focusing only on the disease or condition at issue.
- Medically Reasonable and Necessary Elements. Though the 2020 MPFS provides for the requirements listed in this document, the 2020 MPFS also states that all elements do not necessarily apply every month in order for the codes to be billed, so long as those elements that are medically reasonable and necessary are provided.
- RHCs and FQHCs. RHCs and FQHCs that furnish PCM services will bill the general care management HCPCS code G0511, either alone or with other payable services on an RHC or FQHC claim. The payment rate for HCPCS code G0511 is the average of the national non-facility physician fee schedule payment rate for care management and general behavioral integration codes (CPT codes 99484, 99487, 99490, and 99491) and PCM CPT codes 99424 and 99426.
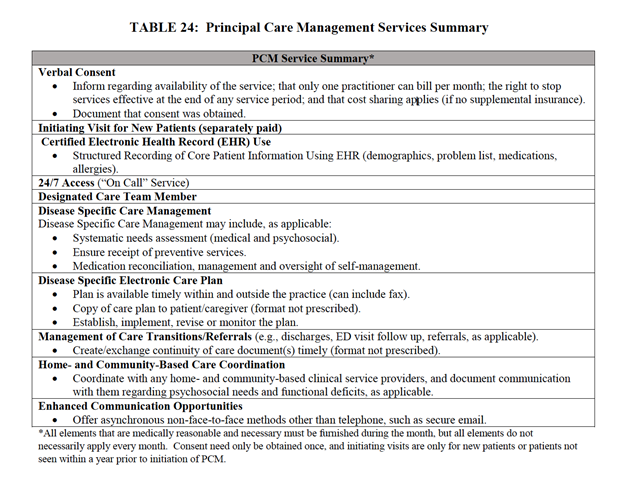
CMS provides the following table on page 424 of the 2020 Rule, laying out in some detail the specific requirements applicable to PCM services:
Supercharge Your Health System or Practice by Leveraging PCM Codes With HealthSnap
The PCM CPT codes are a valuable resource for providers who want to offer their patients the best possible care. HealthSnap is committed to helping our clients use these codes to their fullest potential, and we invite you to schedule a demo with us so that we can show you how easy it is to get started. With HealthSnap’s help, you can provide your patients with the quality care they deserve and improve your practice’s bottom line in the process.






