Value-based care has emerged in recent years as an important approach to delivering healthcare that aligns with the best interests of both the patients and medical providers. It helps drive improved patient outcomes while lowering the costs of healthcare delivery and supporting the provider’s financial bottom line.
In other words, achieving the quadruple aim:
- Improving patient outcomes
- Improving the patient experience
- Improving the provider experience
- Lower the total cost of care
Increasingly recognized as a more effective alternative to the fee-for-service care model, value-based care is creating a win-win for all stakeholders in the healthcare system through programs, such as Remote Patient Monitoring (RPM) and Chronic Care Management (CCM).
Remote Patient Monitoring programs primarily focus on collecting and analyzing physiologic data in near real-time to help care teams remotely track and manage a care plan for a patient’s chronic or acute condition. Chronic Care Management (CCM) typically includes virtual care services offered to Medicare beneficiaries with two or more chronic conditions that are anticipated to last for at least one year or until the end of life.
How RPM and CCM Drives Value-Based Care Delivery

By improving health outcomes and reducing complications and disease progression, value-based care models prove to be more beneficial and cost-effective for patients over time, while at the same reducing the provider’s cost of healthcare delivery, increasing their ability to serve more patients across geographies and demographic segments, delivering on the quadruple aim, and building stronger patient-provider relationships.
Remote Patient Monitoring and Chronic Care Management together can help healthcare providers build a more effective, data-driven process for the delivery of best-in-class care to patients. A survey in 2019 showed that the key barriers to the adoption of value-based care models included difficulties in collecting and reporting patient data, lack of reliable IT infrastructure, and gaps in internal and external interoperability.
RPM and CCM care delivery models address each one of these barriers to make value-based care sustainable for healthcare providers.
How RPM and CCM Lay the Foundation for Value-Based Care
When a healthcare provider leverages an integrated Virtual Care Management solution (interoperable with their Electronic Medical Records) to implement Remote Patient Monitoring and Chronic Care Management programs, they are laying the foundation for value-based care. The same skill sets and resources can be utilized for the implementation of both RPM and CCM programs.
Chronic Condition Management
Care teams can track the variations in patient health data in near real-time, detect developing complications early, track medication compliance, and address an exacerbation of symptoms faster. This helps lower the incidence of readmissions, reduces office visits and ER visits, and improves health outcomes.
More Clinical Time
Chronically ill patients with multiple chronic conditions typically need care from more than one care provider or specialist, and their treatment plans may need frequent adjustments. RPM and CCM programs enable care teams to have more clinical time available to focus on multiple or complex issues that impact care, instead of just the central health concern.
Stronger Relationships
Greater patient involvement and engagement with the care team lead to a stronger relationship of trust and transparency between the patient and the provider. Patients feel more satisfied and have a higher motivation to meet the provider’s expectations in terms of compliance. Care teams are also able to devote more personalized care and attention and work with a greater sense of accountability.
How are RPM and CCM Integrated as Part of a Value-Based Care Model?

CMS originally created incentives for non-face-to-face Chronic Care Management in 2015 and Remote Patient Monitoring in 2018. Thereafter, a rapid acceptance and adoption of RPM and CCM by leading healthcare organizations and patients led to an expansion of the coverage and the rates in order to promote these value-based care technologies.
Both CCM and RPM have received robust endorsement and support from CMS. The resulting revenues via Medicare claims for both these programs are now significant because RPM has been recognized by CMS as supplementary to CCM. Until a few years ago, the successful implementation of CCM was a challenge because of coordination problems among healthcare providers addressing different aspects of the patient’s condition.
At the same time, patients often felt overwhelmed because they have to engage with multiple healthcare providers and face hurdles in complying with different treatment plans or medications prescribed to them. This kind of fragmentation in care delivery adversely affected patient outcomes in many cases, leading to sudden ER visits and re-hospitalizations.
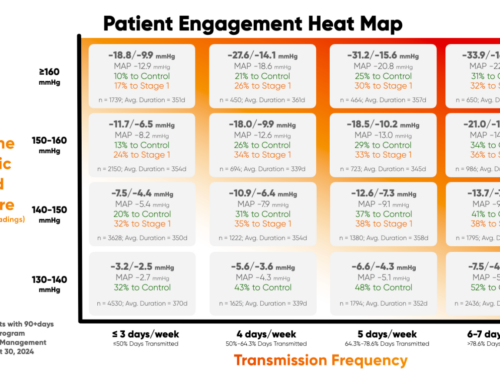
Remote Patient Monitoring medical devices have been able to resolve the fragmentations in care delivery and bridged care gaps because it gives care teams access to near real-time patient data related to multiple chronic conditions. Consider the example of patient requirement management of hypertension. A cellular RPM blood pressure monitoring device can capture accurate and continuous readings of systolic and diastolic blood pressure and transmit them to the care teams.
Any abnormal fluctuations in blood pressure levels of the patient can be detected in near real-time and appropriate preventive care management can be initiated. This reduces the chances of the condition escalating into a medical emergency. This is how a well-organized RPM program can support CCM by giving the care team access to timely patient data insights for proactive care.
CCM and RPM together consolidate care delivery, leading to a number of positive patient outcomes, including:
- Improved patient outcomes through timely detection and medical intervention
- Optimization of patient experience, including better engagement, motivation, and satisfaction
- Lower healthcare costs with fewer ER visits and hospitalizations
- Reduction in the overall stress on the healthcare system
- Greater awareness, education, and compliance among patients and their caregivers
- Additional revenue streams for healthcare providers from RPM and CCM billable reimbursements
RPM and CCM Should Go Hand-in-Hand: A More Effective Care Strategy

By combining RPM and CCM to deliver value-based care, healthcare providers are empowered with a unified care management solution that can be adapted to meet their unique requirements for care delivery. The eligible services of both Remote Patient Monitoring and Chronic Care Management are complementary to each other.
Based on their practice needs, healthcare providers can create an optimized strategy on which services they want to utilize during a particular month. This becomes possible because concurrent billing is allowed for both services for the same time period. As long as there’s no double-counting of the time spent, “stacking” of CCM and RPM is allowed in the same month.
Remote Patient Monitoring can also be used to improve the delivery of Chronic Care Management, particularly for patients with one chronic condition (which does not qualify for CCM reimbursement). In general, both CCM and RPM offer providers, patients, payers, and the complete healthcare ecosystem a more cohesive strategy to improve patient health outcomes as well as financial outcomes for all stakeholders.
RPM is the Technology that Powers CCM to Work Better

While it is clear that CCM and RPM work best hand-in-hand, it is noteworthy that they have their own unique roles and responsibilities. Remote Patient Monitoring is a powerful technology aimed at improving care for patients with chronic conditions, and together they power a data-driven and comprehensive approach to improving outcomes and reducing utilization for high-risk, high-cost populations.
Care providers cannot afford to ignore the critical importance of tracking the patient’s vital signs and mere telephonic communication in absence of continuous patient data is not enough. That makes RPM an important and natural ally of any successful CCM program. In simple words, CCM is the care program, while RPM is the data monitoring designed to make it work more effectively.
It’s notable that Remote Patient Monitoring programs can be utilized not just for care related to chronic conditions, but also for temporary rehab care as well as acute care related to pre-surgery monitoring and post-surgery recovery. Looking at the synergistic power of both RPM and CCM together, it makes sense for healthcare providers to choose an integrated virtual care platform that has the technological capacity and know-how to efficiently optimize each service.
The virtual care services provider should have a demonstrated capability to support robust RPM and CCM care programs for healthcare providers. For medical practices and health systems that are not yet fully leveraging the power of value-based care, now is the opportune time to partner with a leading and trusted vendor for a comprehensive Remote Patient Monitoring program and start reaping the benefits immediately.
Manage Chronic Conditions the Right Way with HealthSnap

HealthSnap’s integrated Virtual Care Management platform is helping improve chronic disease outcomes by delivering continuous, proactive, and remote patient care across high-risk chronic populations. The HIPAA-compliant, HITRUST-certified interoperable solution from HealthSnap ensures compliance, reliability, and security to support care coordination at scale.
Healthcare providers can generate thousands in new revenue per patient annually with HealthSnap’s patented Eligibility Report for RPM billing. Our Virtual Care Management platform is delivering measurable results, with over 70% of the patients enrolled showing improved health outcomes. To learn more about HealthSnap, or to request a demo of our RPM program, call today at 888-780-1872 or click here to schedule a consultation.