Obesity is a serious public health challenge in the US, contributing to a range of chronic diseases, including high blood pressure, diabetes, and cardiovascular diseases. The traditional approaches to weight management, which include diet modification, increased physical activity, and behavioral interventions, have shown varying degrees of success. However, these methods often lack the support systems necessary to sustain long-term weight loss and health improvements.
Virtual Care Management (VCM), encompassing Remote Patient Monitoring (RPM), Chronic Care Management (CCM), and Principal Care Management (PCM), has emerged as an innovative solution to help bridge this gap. These technologies offer ongoing monitoring, a more personalized approach to care, and proactive management, which may significantly improve weight management outcomes.
RPM in Weight Management
Role of RPM in Tracking Weight, Physical Activity, and Other Metrics
Remote Patient Monitoring has emerged as a transformative tool in weight management by enabling the continuous tracking of essential health metrics like weight, physical activity, and other related indicators. A key component of RPM is the use of cellular-enabled scales that automatically transmit data to healthcare providers. These scales allow patients to measure their weight regularly at home, with the data being sent to a central database where it can be monitored by healthcare professionals in near real-time.
This technology may also be integrated with wearable devices that track physical activity, such as steps taken, calories burned, and heart rate. By providing a comprehensive view of a patient’s health, RPM systems facilitate a more nuanced understanding of a patient’s weight management journey. The data collected allows healthcare providers to monitor progress, identify trends, and intervene promptly when necessary, making adjustments to the patient’s treatment plan based on the latest information.
Near Real-Time Weight Monitoring Data Allows for Timely Interventions
One of the critical advantages of RPM is the ability to collect and analyze health data in near real-time. This immediacy allows healthcare providers to respond quickly to any concerning trends in a patient’s weight or physical activity levels. For instance, if a patient begins to gain weight or shows a decline in physical activity, a healthcare provider can intervene by contacting the patient to discuss the issue, offering advice, or adjusting the treatment plan.
This rapid response capability is critical for preventing small setbacks from becoming significant challenges in the patient’s weight management program. Moreover, near real-time data enables a more personalized approach to care, as adjustments can be made promptly to better align with the patient’s current needs and circumstances.

Studies Show the Effectiveness of RPM in Weight Reduction
Numerous studies have demonstrated the effectiveness of RPM in supporting weight loss and overall weight management. Here are some key findings:
-
A 2016 study published in the Journal of Medical Internet Research found that participants who used an RPM program, which included a cellular scale and regular provider feedback, lost significantly more weight over six months compared to those who did not use the RPM program. The study showed that the integration of Remote Patient Monitoring tools into weight management strategies can lead to better outcomes in weight loss efforts.
-
A 2018 study in Obesity Journal evaluated the long-term impact of RPM on weight management in a cohort of obese patients. The study reported that participants who engaged in RPM for a year showed a sustained weight loss of 7% on average, highlighting the potential of RPM in helping patients maintain their weight loss over time.
-
A 2020 study published in the International Journal of Obesity explored the effectiveness of RPM in a clinical setting. The study revealed that patients who regularly transmitted their weight data via RPM experienced an average weight reduction of 8.5 lbs over nine months, compared to a control group with no significant weight change.
Case Studies Demonstrating RPM’s Impact on Sustained Weight Loss
Several case studies have also highlighted the success of Remote Patient Monitoring in helping individuals achieve and sustain weight loss. For example, a healthcare network in the Midwest implemented an RPM program for weight management among its patients. Over 12 months, patients enrolled in the program lost an average of 10 pounds, with many reporting enhanced motivation to maintain their weight loss due to regular feedback from healthcare providers. Another case study from a large urban health system showed that patients who used RPM scales were more likely to adhere to their weight loss goals and reported feeling more accountable for their health outcomes.
RPM Enhances Patient Motivation and Accountability
Remote Patient Monitoring devices have been shown to significantly enhance patient motivation and accountability in weight management programs without relying on weight loss medications. The continuous monitoring and the knowledge that healthcare providers are actively engaged in their progress encourage patients to stay committed to their weight loss goals. Knowing that their data is being reviewed regularly, patients are more likely to adhere to recommended lifestyle changes, such as dietary adjustments, an intensive exercise program, and increased physical activity.

Role of Continuous Feedback in Fostering Healthy Behaviors
Continuous feedback is another critical element of Remote Patient Monitoring that fosters healthy behaviors. As patients receive regular updates and encouragement from their healthcare providers, they are more likely to feel supported and empowered to make positive changes. This feedback loop helps to reinforce healthy habits and provides patients with the necessary tools and confidence to sustain their weight management efforts over the long term.
By integrating Remote Patient Monitoring into weight management programs, healthcare providers can offer more personalized, effective, and timely interventions, ultimately leading to better health outcomes for patients struggling with weight management.
CCM in Weight Management
Integration of Weight Management into Broader Chronic Disease Care
Chronic Care Management is a comprehensive approach to managing chronic diseases, including obesity and related conditions like hypertension, diabetes, and cardiovascular disease. CCM integrates weight management into the broader framework of chronic disease care by addressing weight as a critical factor in overall health. Patients enrolled in CCM programs often have multiple chronic conditions, and effective weight management is essential in mitigating the risks associated with these conditions.
In CCM, weight management is not treated as an isolated goal but as a component of a patient’s overall health strategy. This integration allows healthcare providers to monitor and address weight issues alongside other chronic conditions, ensuring that weight loss or maintenance efforts are aligned with the patient’s broader health objectives. By incorporating weight management into chronic disease care, CCM helps patients achieve more sustainable health outcomes.
The Structured Approach of CCM
CCM programs offer a structured approach to weight management, which includes regular check-ins, obesity treatment, medication management, patient’s blood pressure monitoring, and the coordination of care among various healthcare providers.
-
Regular Check-ins: Patients have scheduled interactions with their healthcare team, allowing for continuous monitoring of their weight and other health metrics. These check-ins can be used to assess progress, discuss challenges, and adjust treatment plans as needed. Regular communication ensures that patients remain engaged and focused on their weight management goals.
-
Medication Management: For patients with chronic conditions, medication plays a critical role in their overall health. CCM ensures that medication management is tailored to each patient’s needs, with careful consideration of how medications might impact weight. Adjustments can be made to minimize weight gain or support weight loss, especially in patients dealing with obesity-related conditions.
-
Coordination of Care: CCM involves the collaboration of various healthcare professionals. This coordination ensures that all aspects of a patient’s health are addressed, and that weight management strategies are consistent across all areas of care. By having a cohesive care plan, patients receive the most effective and personalized treatment possible.

Evidence of CCM’s Impact on Weight Management
Numerous studies have demonstrated the effectiveness of CCM in managing obesity-related conditions:
-
A 2018 study in the Journal of General Internal Medicine found that patients enrolled in CCM programs had better outcomes in managing obesity and related conditions compared to those who received standard care. The study highlighted that regular monitoring and coordinated care significantly improved patients’ ability to achieve and maintain a healthy weight.
-
A 2020 research article in Obesity Reviews analyzed the long-term impact of CCM on weight management in patients with multiple chronic conditions. The findings showed that patients in CCM programs experienced sustained weight loss over a three-year period, which was associated with better control of other chronic diseases such as diabetes and hypertension.
-
A 2021 study published in the American Journal of Managed Care examined the role of CCM in weight management among Medicare beneficiaries. The study concluded that patients who participated in CCM had a 25% higher likelihood of achieving significant weight loss compared to those not in CCM, underscoring the program’s effectiveness in managing obesity-related conditions.
Long-Term Outcomes Associated with CCM in Weight Management
Long-term studies have shown that CCM can lead to sustained weight loss and improved management of obesity-related conditions. Patients in CCM programs often achieve and maintain weight loss over extended periods, which is critical for the prevention of complications related to obesity. This sustained weight management contributes to the long-term control of chronic diseases, reducing the risk of heart disease, stroke, and other obesity-related health issues.
Empowering Patients to Make Healthier Lifestyle Choices
A critical component of CCM is patient education, which empowers individuals to make informed decisions about their health. Through education, patients learn about the importance of diet, exercise, and other lifestyle factors in managing their weight. CCM programs often include personalized educational materials and resources that help patients understand how their choices impact their overall health. This knowledge enables patients to take an active role in their weight management journey, making healthier lifestyle choices that support long-term success.

Role of Self-Management in Achieving Weight Loss
Self-management is a key factor in achieving and maintaining weight loss in CCM programs. Patients are encouraged to take responsibility for their health by actively participating in their care plan. This involves regular self-monitoring of weight, adherence to prescribed treatments, and making necessary lifestyle adjustments. The structured support provided by CCM helps patients develop the skills and confidence needed to manage their weight independently, leading to more sustainable outcomes.
PCM in Targeted Weight Management
How PCM Provides Focused Care for Weight Management
Principal Care Management offers a customized approach to weight management by focusing on the specific needs of individuals dealing with obesity or related conditions. Unlike general chronic care management, PCM zeroes in on a single chronic condition—such as obesity—allowing healthcare providers to develop highly personalized care plans. This targeted approach ensures that patients receive the most appropriate interventions and support needed for effective weight management.
PCM’s personalized care involves in-depth assessments of a patient’s health status, lifestyle, and weight management goals. Health care providers use this information to create customized dietary and exercise plans, ensuring that the recommendations are both realistic and effective. These individualized plans take into account factors such as the patient’s metabolic rate, existing comorbidities, and personal preferences, making it easier for patients to adhere to the prescribed regimen.
Development of Individualized Dietary and Exercise Plans
The cornerstone of PCM in excess weight management is the creation of individualized dietary and exercise plans. These plans may be designed based on a comprehensive understanding of the patient’s health needs and goals.
-
Dietary Plans: PCM allows for the development of tailored dietary plans that align with the patient’s nutritional needs, food preferences, and lifestyle. These plans often focus on balanced nutrition, portion control, and the inclusion of specific nutrients that can help in weight management and overall health improvement.
-
Exercise Plans: Exercise is a critical component of weight management, and PCM ensures that the physical activity recommendations are personalized. This might involve creating exercise routines that cater to the patient’s fitness level, physical limitations, and time constraints, making it more likely that the patient will stick to the plan and see results.
The ongoing monitoring and adjustment of these plans are also integral to PCM. As patients progress, their dietary and exercise plans can be modified to reflect changes in their weight, health status, and any challenges they may face, such as weight loss plateaus.
Evidence Showing the Effectiveness of PCM in Weight Reduction
Research has shown that PCM can lead to significant weight reduction, particularly when it is focused on personalized care and continuous monitoring. Some of the key studies include:
-
A 2019 study in the American Journal of Managed Care found that patients receiving PCM for weight management had a 30% greater reduction in body mass index (BMI) compared to those receiving standard care. The study highlighted the role of personalized care in achieving substantial weight loss.
-
A 2020 study published in Obesity demonstrated that patients enrolled in PCM programs for obesity management lost an average of 10% of their body weight over six months, with many maintaining or continuing to lose weight over a year.
-
A 2021 meta-analysis in the Journal of Clinical Endocrinology & Metabolism analyzed several PCM-based interventions and concluded that PCM was associated with a significant reduction in weight and improvement in obesity-related comorbidities such as type 2 diabetes and hypertension.
Benefits of PCM in Reducing Obesity-Related Health Risks
PCM’s focus on sustained weight management has long-term benefits in reducing obesity-related health risks. By maintaining weight loss, patients can significantly lower their risk of developing conditions such as cardiovascular disease, type 2 diabetes, and certain cancers. PCM also helps in managing existing conditions more effectively, leading to better overall health outcomes and reduced healthcare costs.

Role of PCM in Addressing Weight Loss Plateaus and Weight Regain
One of the common challenges in weight management is the occurrence of weight loss plateaus, where patients stop losing weight despite continuing their diet and exercise routines. PCM plays a critical role in overcoming these challenges by providing continuous monitoring and timely interventions.
-
Addressing Plateaus: PCM allows healthcare providers to identify plateaus early and adjust the patient’s care plan accordingly. This might involve altering the dietary plan, increasing the intensity or variety of exercises, or addressing underlying issues such as metabolic adaptation.
-
Preventing Weight Regain: Weight regain is another significant challenge, especially after initial success in weight loss. PCM’s structured approach, which includes regular follow-ups and adjustments to care plans, helps patients maintain their weight loss over the long term. Continuous support and education help patients make sustainable lifestyle changes, reducing the likelihood of regaining the lost weight.
PCM’s comprehensive and personalized approach to weight management not only facilitates significant weight loss but also ensures that patients can maintain their progress and improve their overall health in the long term.
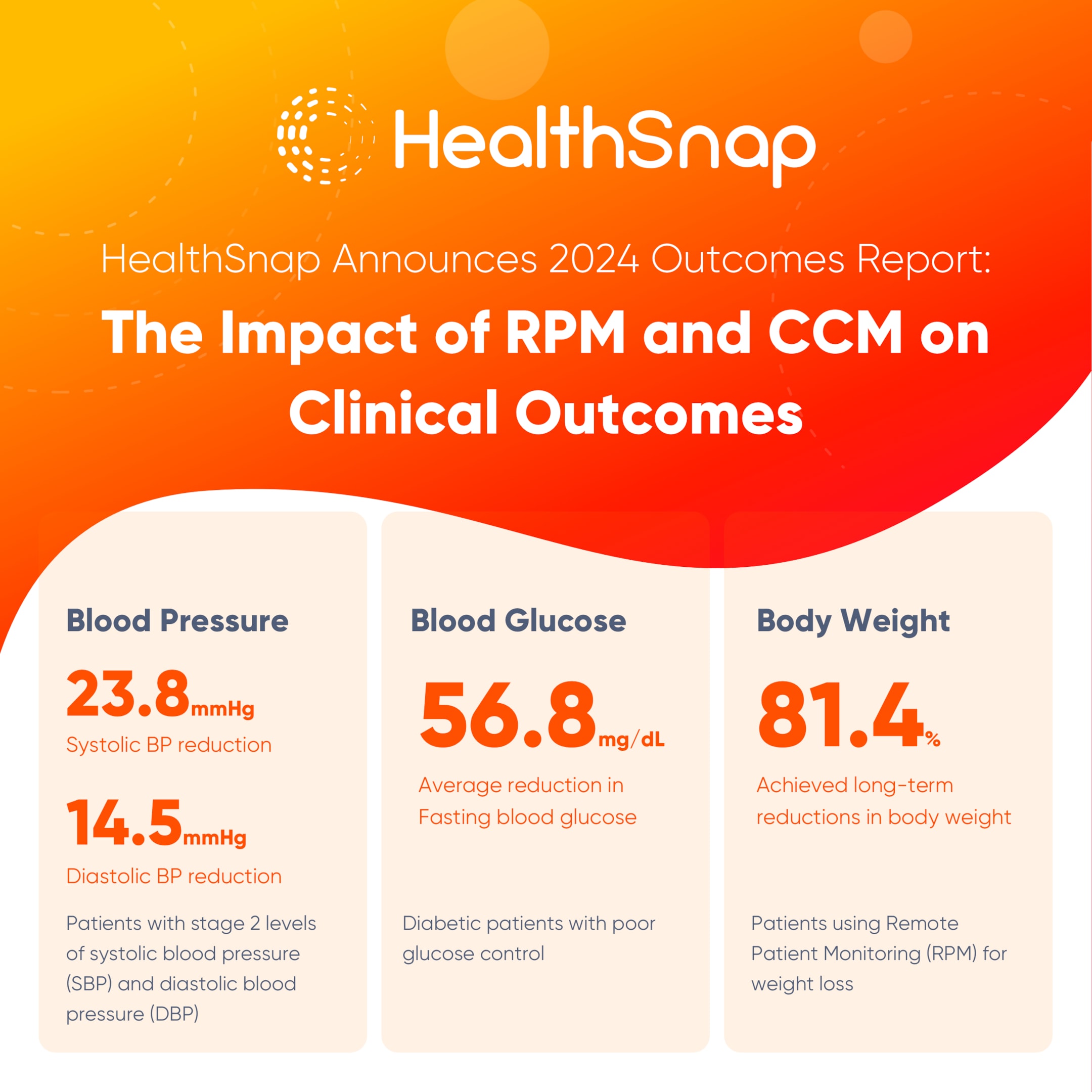
HealthSnap 2024 Healthcare Outcomes Report
HealthSnap’s 2024 Clinical Outcomes Report reveals that Remote Patient Monitoring and Chronic Care Management programs are effective in managing chronic conditions like obesity. Patients who engage more frequently and stay in the program longer experience greater health improvements, including significant reductions in body weight. These improvements not only enhance patient health but also reduce healthcare costs and make healthcare more accessible to underserved populations.
Methodology & Analysis of Body Weight RPM for Managing Obesity
HealthSnap study analyzed the effects of RPM on weight management among 494 patients specifically monitored for obesity. The results showed significant clinical improvements:
-
Average Weight Loss: Patients lost an average of 8.8 lbs over approximately 324 days.
-
Success Rate: 81.4% of these patients successfully lost weight.
Relationship Between RPM Program Duration & Transmission Index and Management of Obesity
When analyzing the data by program duration:
-
Longest Participation (Quartile 4: 403-1071 days): Patients lost over 300% more body weight compared to those in Quartile 1 (90-185 days), translating to 6.7% vs. 1.8% of their total body mass.
When comparing across quartiles of data transmission:
-
Highest Data Transmission (Quartile 4: 87.4-100%): Patients experienced a greater decrease inweight compared to those who transmitted data less frequently, highlighting a significant correlation between engagement and weight loss outcomes. This suggests that longer participation in the RPM program and consistent data transmission are key factors in successful weight management.
Give Your Healthcare Practice the Power of HealthSnap’s VCM Platform
HealthSnap’s integrated Virtual Care Management Platform empowers you to deliver proactive, continuous, and secure virtual care management programs to your high-risk, chronic patient population. Whether you are a provider group looking to strengthen your care team or a health system aiming to revolutionize chronic disease management, HealthSnap provides effective virtual care management programs and tools. Call us at 888-780-1872 or contact us online to schedule a consultation or a demo with one of our Specialists.






