Healthcare delivery in recent years has been profoundly reshaped by the evolution of remote care, which encompasses dynamic telehealth and virtual care management programs like Remote Patient Monitoring (RPM) and Chronic Care Management (CCM). In this article, we reflect on the historical trajectory of these transformative innovations and explore their current state.
Remote care has traversed a remarkable journey, with roots dating back to the late 19th century and blossoming into a unique web of telecommunication and information technologies. The fusion of medical expertise and digital innovation has not only addressed historical challenges in healthcare access but has also set the stage for a future where the boundaries of traditional care can be extended.
The Evolution of Remote Care
The evolution of remote care has been remarkable, driven by the imperative to bridge gaps in healthcare access and enhance the management of chronic diseases.
Home- and Community-Based Care
Historically, the roots of home-based care can be traced back to an 1879 Lancet article that envisioned using the telephone to reduce unnecessary office visits, setting the stage for telehealth innovations. Fast forward to the 21st century, and we witness a convergence of advanced telecommunication and information technologies in the pursuit of addressing healthcare disparities. The emphasis on home- and community-based care arises from the recognition that the traditional episodic office-based model, often insufficient for managing chronic diseases, needed a paradigm shift toward more continuous and personalized care.
One significant stride in this evolution is the utilization of telecommunication and information technology to redistribute knowledge and expertise. As chronic diseases account for a substantial portion of healthcare expenditures, there is a pressing need to manage them effectively. The Veterans Affairs (VA) care management program, developed over a decade ago, exemplifies a successful approach. This program offered personalized education, monitoring, and feedback at home through a remote disease management support team. The integration of technologies into chronic disease care management has shown promising outcomes, including reductions in hospitalizations, readmissions, lengths of stay, and costs, alongside improvements in physiologic measures and patient satisfaction.
Looking ahead, the era of home- and community-based care in remote health is poised for further advancements. The future envisions a proliferation of laptop-based, tablet-based, and wearable devices for physiological monitoring. Companies are exploring the development of wearable wireless devices that amalgamate various functions, such as accelerometers, stethoscopes, and electrocardiograms, enabling continuous monitoring. Moreover, innovations may extend to devices like watches or rings that measure blood pressure and heart rate.

Notably, policy changes emerge as a critical factor in propelling the evolution of home- and community-based care in remote health care. Ensuring the integration and acceptance of these technologies into the broader healthcare system requires a regulatory framework that supports their utilization. As the journey of remote care continues to unfold, stakeholders must collaborate to surmount these challenges and pave the way for a future where home- and community-based care seamlessly integrates technology to provide accessible, efficient, and patient-centric healthcare solutions.
Office-Based Telemedicine
Telemedicine’s historical roots in clinical settings can be traced back to 1906 when the inventor of the electrocardiogram published a paper on the telecardiogram. Since then, the path of office-based telemedicine has been marked by milestones, with radio communication in the 1920s providing medical advice to clinics on ships and Alaska emerging as a model for telemedicine development.
In the modern era, high-definition telemedicine units equipped with peripheral devices for physical examination have become commonplace. Based on this, the proliferation of various units with proprietary communication methods has underscored the need for standardized communication protocols to ensure interoperability.
A significant advancement in office-based telemedicine is the adoption of store and forward (S&F) or asynchronous technologies. This approach has proven valuable in various medical fields, such as ophthalmology, optometry, teledentistry, dermatology, and psychology.
For instance, non-mydriatic cameras have been employed in ophthalmology to conduct retinal screenings in diabetics without dilating the eyes, contributing to increased screening rates. Teledermatology has demonstrated high rates of agreement between in-person and remote diagnoses, offering satisfaction and timely access to care. However, the broader adoption of teledermatology has faced challenges, primarily related to reimbursement issues.
Despite these advancements, office-based telemedicine faces a set of challenges and opportunities. The integration of nontraditional providers and community clinical expertise is a key consideration. Determining the optimal use of new telehealth models and improving interfaces through technologies like high-definition or three-dimensional images remain ongoing endeavors. Additionally, the role of less costly equipment, such as handheld devices like cellular-based smartphones, needs deeper recognition.

Looking ahead, the future of office-based telemedicine holds promises of continued innovation. The integration of telemedicine into electronic health records is expected to streamline workflows and enhance coordination of care. Wearable devices are likely to play a more significant role, enabling patients to actively participate in their healthcare through continuous monitoring. The ongoing development of evidence-based standards for care and the establishment of reimbursement models that support telemedicine in rural and remote communities will be essential for sustainable growth.
Ancillary Telemedicine Services
The evolution of remote care has extended its transformative reach into ancillary telemedicine services, marking a significant chapter in the ongoing revolution of healthcare delivery. Teleradiology, telepathology, and telepharmacy have emerged as pivotal components, leveraging technology to overcome geographical barriers, enhance diagnostic capabilities, and improve medication management.
Teleradiology
For over six decades, teleradiology has been at the forefront of remote care. Originally utilizing film and later transitioning to direct digital capture, this service allows medical images to be transmitted and read in distant locations. The promotion of the Digital Imaging and Communications in Medicine (DICOM) standard has been instrumental in ensuring seamless data transmission. Studies have highlighted the positive impact of teleradiology, reducing transports for head injuries out of rural areas and significantly affecting diagnosis and treatment plans.
Telepathology
While less common than teleradiology, telepathology has witnessed substantial growth with the digitization of pathology slides. Overcoming challenges related to large file sizes, innovative models now allow images to be viewed remotely without the need for physical transfer. Studies have demonstrated the value of telepathology, with specialist pathologists, via telemedicine, outperforming on-site staff pathologists in terms of precision of diagnosis.
Telepharmacy
The practice of pharmacy over a distance, telepharmacy, has been facilitated by computerized physician order entry and remote review. The integration of video consultations enables comprehensive remote pharmacy visits. Research studies have showcased the significant impact of telepharmacy, with one study reporting savings of 27,000 miles of travel for 47 cancer patients and another revealing a reduction of medication errors by remote pharmacists in rural hospitals.
Hospital-Based Telemedicine
From pioneering closed-circuit television consultations in the late 1950s to contemporary applications in stroke care and intensive care units (ICUs), hospital-based telemedicine has become a critical component of modern healthcare.
Historical Milestones
One of the earliest uses of hospital-based telemedicine occurred in the late 1950s, establishing a closed-circuit television link between the Nebraska Psychiatric Institute and Norfolk State Hospital for psychiatric consultations. Over the years, the focus on hospital-based telemedicine has grown, particularly in stroke care and ICUs. The efficacy of telemedicine in stroke care has been demonstrated through high-quality imaging, enabling remote examination and consultation. In ICUs, studies indicate associated reductions in length of stay, mortality rates, and overall healthcare costs.
Devices and Applications
Hospital-based telemedicine has not only found its place in large medical facilities but has also extended its reach to inpatient settings and skilled nursing facilities. The integration of telemedicine in nursing homes has shown strong evidence of clinical benefit and savings. Furthermore, families and nursing home personnel have expressed positive feedback regarding telepsychiatry for geropsychiatric care. The introduction of telesurgery, albeit on a small scale, demonstrates the potential for leveraging experts’ technical skills and knowledge through remote care.
Challenges and Future Prospects
While hospital-based telemedicine has witnessed considerable growth, challenges persist. Determining the essential elements of tele-ICU that contribute to its effectiveness remains an area of exploration. The expansion of hospital-based telemedicine has predominantly occurred with for-profit companies offering specialized care to well-resourced hospitals. Bridging the gap to make these services accessible to smaller hospitals, either through private or public means, remains a challenge. As payers increasingly focus on reducing readmissions, the utilization of telemedicine in skilled nursing facilities is anticipated to rise, presenting a new frontier for hospital-based remote care.
Remote Patient Monitoring: A Historical Journey
The historical journey of remote patient monitoring (RPM) represents the innovative spirit that has shaped the modern healthcare industry. Rooted in pioneering moments that date back over a century, RPM has evolved from rudimentary concepts to sophisticated technologies, offering new dimensions in medical care and healthcare services and management.
Pioneering Moments
March 7, 1876 — Alexander Graham Bell’s Telephone Patent
The inception of RPM can be traced back to Alexander Graham Bell’s revolutionary invention of the telephone. Granted a patent on March 7, 1876, Bell’s creation laid the groundwork for electronic communication. Little did he know that this invention would be a catalyst for Remote Patient Monitoring, enabling the transmission of health-related data across distances.
Early 1900s — Development of Radio Communication
In the early 1900s, lacking the infrastructure for widespread telephone adoption, radio communication emerged as an alternative means of transmitting information. This development set the stage for the evolution of remote patient monitoring, as healthcare providers began to explore ways to leverage radio technology for medical purposes.
1948 — Official Implementation of Telehealth
A significant milestone in the history of Remote Patient Monitoring occurred in 1948 when physicians in West Chester, Pa., sent radiology images 24 miles over a telephone line for review and consultation with another physician in Philadelphia. This marked the official implementation of telehealth, as medical services professionals utilized technology to remotely share and interpret diagnostic images.
1959 — Transmission of Neurological Exams
The late 1950s saw doctors normalizing and relying on the telehealth concept by transmitting neurological exams for consultation. This development expanded the scope of Remote Patient Monitoring, allowing healthcare providers to remotely assess and diagnose neurological conditions, paving the way for future advancements in neurological and mental health services.
1961 — Alan Shepard’s Monitoring in Space
A groundbreaking moment in the history of RPM occurred in May 1961 when Alan Shepard, the first American in space, was monitored during his flight. The National Aeronautics and Space Administration (NASA) utilized early electrocardiogram (EKG) technology, a thermometer, and a respiration sensor in his microphone to monitor Shepard’s health remotely. This marked the birth of remote patient monitoring, as biometric data was transmitted from space, showcasing the potential for monitoring individuals in real-time, even in extreme environments.
1967 — EKGs Over Telephone Wires
In 1967, health professionals took a step further by sending electrocardiograms (EKGs) over telephone wires. This development expanded the applications of remote patient monitoring to cardiac care, allowing health system teams to remotely monitor heart activity and make informed decisions based on the transmitted data.

Technological Milestones in RPM Services
From early technological breakthroughs to the sophisticated remote multiple medical devices and telehealth services of today, RPM has continually evolved, improving access as well as quality of care.
1970s — The Papago Indian Reservation RPM Program
In the 1970s, the Papago Indian Reservation in Arizona became a pioneering site for the development and deployment of the first official remote patient monitoring program for Earthside patients. Although the program faced complications and was discontinued in 1977, the knowledge gained during this initiative was leveraged by NASA in its space technology program. This marked an early attempt at integrating technology into patient care beyond traditional healthcare settings.
1980 — Transmission of X-Ray Images
The 1980s saw a significant leap in RPM with health professionals normalizing the transmission of x-ray images over distances. This technological advancement allowed for the remote interpretation of diagnostic images, enabling specialists to provide insights and recommendations without the need for physical presence. This marked a key development in expanding the scope of RPM beyond simple data transmission.
1982 — Introduction of the First Wearable Biometric Sports Watch
In 1982, the introduction of the first wearable biometric sports watch showcased the potential for integrating monitoring technology into patients’ daily lives. This watch, incorporating basic EKG technology and a radio chest strap, enabled athletes to measure heart rate and activity levels. While initially designed for sports, this laid the groundwork for the incorporation of wearables into Remote Patient Monitoring.
1990s — Development of Cellular Communication
The 1990s witnessed the development of cellular-based communication technology. Although its initial applications were not healthcare-focused, the introduction of cellular-based communication laid the groundwork for the future of RPM. This technology enabled seamless communication between cellular devices, paving the way for the development of remote health monitoring devices.
2019 — Changes to CPT Codes for RPM
In 2019, changes to Current Procedural Terminology (CPT) codes marked a significant policy shift, making RPM one of the most lucrative Medicare care management programs. While the adoption was initially slow, these changes set the stage for increased reimbursement and incentivized medical professionals to embrace RPM as a viable and financially rewarding method of care.
2020 — The COVID-19 Pandemic and RPM Surge
The COVID-19 pandemic in 2020 served as a catalyst to facilitate Remote Patient Monitoring. With healthcare systems grappling with the need for remote care solutions, the federal government and private payers expanded coverage of RPM. A surge in the usage of RPM tools and services was observed, with more than 23 million US patients benefiting from remote monitoring in 2020 alone.
Recent Developments and Challenges in Remote Patient Monitoring
In the ongoing historical journey of RPM, recent years have witnessed significant developments and encountered notable challenges, impacting the path of this innovative healthcare approach.
2019 — Policy Changes and Recognition
The year 2019 marked a pivotal moment for RPM with changes to Current Procedural Terminology (CPT) codes, elevating its status as one of the most lucrative Medicare care management programs. This shift in policy not only reflected a growing recognition of the value of remote patient monitoring but also set the stage for increased adoption by healthcare providers. The promise of enhanced reimbursement acted as a catalyst, encouraging the integration of RPM into care strategies.
2022 — Adoption Challenges Persist
Despite the growing recognition and appreciation for remote patient monitoring, a 2022 poll by the Medical Group Management Association revealed that only 25% of practices offered RPM. This discrepancy between recognition and adoption suggests persistent challenges in implementing and scaling RPM programs. Barriers may include technological readiness, workforce training, and organizational resistance to change.
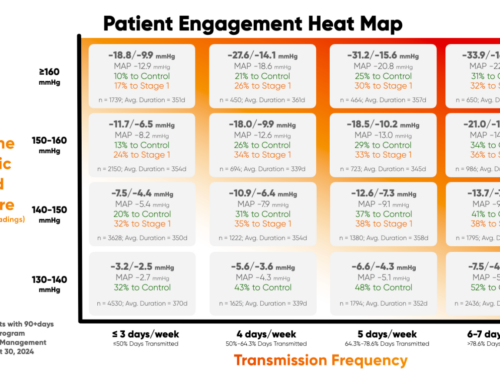
Trends in Patient Engagement and RPM Technology
Recent developments in RPM have seen a heightened focus on patient engagement and the integration of wearable technology. Empowering patients with user-friendly devices that actively involve them in their healthcare journey has become a priority. Cellular-based RPM devices equipped with sensors for monitoring vital signs, physical activity, and chronic condition health metrics are increasingly being incorporated into RPM strategies, promising more comprehensive and personalized care.
Data Security and Interoperability Challenges
As RPM relies heavily on the transmission and analysis of sensitive health data, ensuring robust cybersecurity measures has become an important concern. The need for standardized interoperability across various devices and platforms poses another challenge. Establishing a seamless flow of data between different components of the healthcare ecosystem remains crucial for the success and scalability of RPM programs.
Future Prospects of Remote Care
The future prospects of remote care hold immense promise as technological advancements, changing healthcare landscapes, and evolving patient preferences converge to reshape the way healthcare is delivered. Here are key areas where remote care is expected to flourish in the coming years:
Advanced Monitoring Technologies
The continuous evolution of monitoring technologies is set to redefine remote care. Wearable devices, equipped with sophisticated sensors, will play a pivotal role in monitoring vital signs, activity levels, and even detecting early signs of various health conditions. These advancements will empower individuals to actively participate in their healthcare, promoting preventive measures and early intervention.
Artificial Intelligence (AI) and Predictive Analytics
The integration of artificial intelligence and predictive analytics into remote care systems will revolutionize healthcare delivery. AI algorithms will analyze vast amounts of patient data to identify patterns, predict health outcomes, and provide personalized recommendations. This proactive approach will enable healthcare providers to intervene before issues escalate, improving patient outcomes and reducing the burden on healthcare systems.
Telemedicine and Virtual Consultations
Telemedicine, encompassing virtual consultations and remote visits, is positioned for significant expansion. Improved connectivity, enhanced video conferencing capabilities, and secure communication platforms will contribute to the widespread adoption of virtual care. Patients will have increased access to healthcare professionals from the comfort of their homes, reducing the need for physical visits, especially for routine check-ups and follow-ups.
Remote Chronic Disease Management
Remote care will play a crucial role in the management of chronic diseases. Tailored interventions, continuous monitoring, and personalized care plans delivered remotely will empower individuals with chronic conditions to better manage their health. This approach not only improves patient outcomes but also reduces the strain on healthcare resources associated with frequent hospital visits.

Expanded Scope in Mental Health Care
The future of remote care will witness an expanded focus on mental health. Virtual mental health consultations, remote therapy sessions, and digital mental health tools will become integral components of remote care strategies. This shift is particularly critical in addressing the growing global awareness of mental health challenges and the need for accessible, stigma-free support.
Collaborative and Integrated Care Models
Remote care will increasingly be integrated into collaborative care models. Interdisciplinary teams, including primary care physicians, specialists, nurses, and mental health professionals, will collaborate seamlessly through interconnected digital platforms. This integrated approach ensures holistic and coordinated care for patients, fostering better communication and information sharing among healthcare providers.
Focus on Patient Engagement and Education
Future remote care strategies will prioritize patient engagement and education. Interactive platforms, mobile applications, and personalized health portals will empower individuals to actively participate in their health management. Educational resources and real-time feedback mechanisms will enhance health literacy and promote healthier lifestyle choices.
Data Security and Privacy Measures
As remote care relies heavily on the exchange of sensitive health data, the future will see heightened emphasis on data security and privacy measures. Robust encryption, secure communication channels, and compliance with healthcare data protection regulations will be paramount to instill trust among both healthcare providers and patients.
The Leader in Virtual Care Management Solutions
Achieve your goals in providing affordable and accessible patient-centric care with HealthSnap, your partner in integrated Virtual Care Management. Our innovative Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) programs are designed to enhance care delivery. By seamlessly integrating into your clinical workflows, HealthSnap empowers you to monitor patients’ health metrics in near real-time, ensuring proactive and personalized care.
To schedule a free demo of our RPM and CCM programs, call us today at 888-780-1872 (Ext. 3) or schedule time with one of our specialists.