The Centers for Medicare & Medicaid Services (CMS) issued its highly anticipated Proposed Medicare Physician Fee Schedule for the calendar year 2024 on July 13, 2023. This year’s iteration of the Proposed Rule arrived later than usual, a likely result of its substantial content encompassing significant adjustments and clarifications in the provision of services post the conclusion of the COVID-19 Public Health Emergency (PHE) on May 11th.
Alongside revised considerations for modifications to the Medicare Telehealth Services List and further extensions of telehealth flexibilities, the Proposed Rule bears noteworthy implications for virtual care and care management services beyond the scope of telehealth, including services like Remote Physiologic Monitoring (RPM) and Remote Therapeutic Monitoring (RTM).
In this guide, we will provide an overview of pivotal components within the Proposed Rule concerning RPM, RTM, and other aspects of virtual care management services. This guide also outlines the CMS Medicare challenges and opportunities that stakeholders in this field might encounter.
CMS Proposes “Clarifications” for Remote Monitoring Services
Within the Proposed Rule, CMS presents a series of clarifications pertaining to the appropriate utilization of Remote Patient Monitoring (RPM) and Remote Therapeutic Monitoring (RTM) services. Among these clarifications, some reaffirm previously held positions, one comes as a pleasant surprise, and another is somewhat disconcerting.
This move prompts CMS to actively seek general feedback from stakeholders, with an aim to gather insights for the ongoing development of payment policies governing remote monitoring services eligible for separate payment under the present Physician Fee Schedule (PFS).
RPM and RTM Coverage for FQHCs and RHCs
At present, FQHCs (federally qualified health centers) and RHCs (rural health clinics) are unable to bill for RPM and RTM codes, as these services are considered part of the comprehensive rate encompassing these facilities’ programs’ offerings.
In 2019, CMS took a step to differentiate chronic care management (CCM) from the all-inclusive bundle, allowing FQHCs to independently bill for CCM using the general care management HCPCS code G0511. This change was positively received within the health system, sparking expectations that Remote Patient Monitoring (RPM) would soon follow in obtaining a distinct code.
Although the anticipated timeline was extended, the awaited change is finally on the horizon for 2024. CMS’s proposal for 2024 suggests incorporating RPM and RTM into the G0511 code. This aligns with long-standing advocacy and is a welcome development. If this proposed alteration is ultimately approved, G0511 for 2024 will encompass:
-
Chronic Care Management (CCM)
-
Principal Care Management (PCM)
-
Behavioral Health Integration
-
Chronic Pain Management
-
Remote Therapeutic Monitoring (RTM)
-
Remote Physiological Monitoring (RPM)
However, this proposed rule change carries some ambiguity and peculiarities. Currently, an FQHC is limited to billing one G0511 per month, regardless of the number of care management services delivered. Under this new proposal, it appears that both codes tied to a calendar month (e.g., CCM) and those associated with a rolling 30-day period (e.g., RPM device) would fall under the single-unit-per-month G0511 code.
In this scenario, where billing is feasible for either device readings or care management time each month, a choice needs to be made. Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) must strategize their approach to this situation. Given that G0511’s value will be marginally reduced to accommodate the new codes, providing non-billable services might not be economically viable.
Simultaneously, this change implies that Federally Qualified Health Centers can receive enhanced reimbursement compared to other clinics solely for capturing device measurements without dedicating any care management time.
Distinguishing Remote Monitoring for New and Established Patients
CMS references the 2021 MPFS Final Rule as a reminder that the conclusion of the PHE necessitates the reinstatement of the requirement that RPM and RTM services be rendered solely to “established patients.” However, individuals who initially received remote monitoring services during the PHE, when this requirement was waived, are now categorized as “established patients.”

The “16 Days of Data” Mandate
Despite repeated pleas from stakeholders for a reevaluation, CMS maintains its stance that remote “monitoring must transpire over a minimum of 16 days within a 30-day timeframe.” This slightly differs from its prior stance, which called for 16 days of data transmissions rather than continuous “monitoring” within a 30-day period.
This requirement poses a challenge for monitoring patients and conditions that could potentially benefit from less than 16 days of data transmission. What’s more concerning is CMS’s assertion that this requirement extends to CPT Codes 98980 and 98981, which cover RTM treatment management services. Previously, this requirement was only applicable to device supply and patient education/setup codes.
RPM and RTM in Conjunction with Other Virtual Care Management Services
The Proposed Rule expresses CMS’s intent to provide practitioners with maximum flexibility when selecting the appropriate combination of care management services. This suggests that RPM or RTM (but not both) may be billed concurrently with code sets for services like Chronic Care Management (CCM), Transitional Care Management (TCM), Behavioral Health Integration (BHI), Principal Care Management (PCM), and Chronic Pain Management (CPM). Based on this, the condition is that no time allocated to one service is counted twice for another service.
Can RPM and RTM Be Billed for the Same Patient or Not?
In confirming the possibility of billing RPM or RTM (but not both) concurrently with other care management services, the Proposed Rule asserts that it proposes to clarify that RPM and RTM should not be billed simultaneously. This is to ensure that time is not duplicated through concurrent billing of RPM and RTM services. Moreover, the Rule acknowledges situations in which the same patient receives both RPM and RTM services, possibly using multiple monitoring devices.
In such cases, the Rule refers to existing regulations, particularly those established when introducing the RPM code family. This suggests that services associated with all medical devices can be billed by a single practitioner, once per patient within a 30-day period, as long as at least 16 days’ worth of data have been collected.
This clarification might appear contradictory, unless CMS is suggesting that different practitioners can order RPM and RTM for the same patient, allowing for concurrent billing. Additional clarification in the Final Rule would be advantageous.
Distinct Compensation for Global Surgery Periods
CMS federal government website now officially clarifies that RPM or RTM services can be provided and reimbursed independently of global services payments for surgeries, provided all requisites for global service and any other service during the global period are fulfilled.
Designating RPM as “Primary Care Services” within the Medicare Shared Savings Program
CMS presents a proposition to classify CPT codes 99457 and 99548 as primary care services within the Medicare Shared Savings Program (MSSP), aimed at determining beneficiary assignments to an MSSP Accountable Care Organization (ACO).
Solicitation of Information on Digital Therapies, RPM, and RTM
The Proposed Rule incorporates a broad request for information from healthcare providers and other stakeholders, with the objective of gaining deeper insights into the challenges and prospects associated with coverage, access and payment policies.
This request pertains especially to the roles of practitioners and staff involved in furnishing RPM and RTM services, the practical application of these services in clinical practice, experiences related to coding and payment policies, challenges concerning claims processing, the need for additional practitioner education, and guidance regarding remote monitoring, and potential avenues for future rulemaking in the realm of remote monitoring services.
Furthermore, CMS displays interest in understanding the potential interplay between RTM for Cognitive Behavioral Therapy and other digital CBT services. The Rule acknowledges past commenters who have supported the notion of a generic RTM device code similar to the generic supply of device code for RPM, and it seeks feedback on the pros and cons of implementing such a code, along with thoughts on how its valuation should be approached.
Notable Insights
The proposed separate reimbursement for RPM and RTM services when offered by FQHCs and RHCs marks a significant achievement for providers, patients, and digital health companies. Additionally, the clarification that RPM and RTM services can be billed separately when provided within the context of a global surgical period is another substantial victory.

On the flip side, CMS remains resolute in its position that a monitoring duration of 16 days’ worth of data is necessary for specific RPM and RTM codes to be eligible for billing, despite indications that fewer days of data transmission can yield the benefits and improved patient outcomes.
The Proposed Rule allows numerous opportunities for stakeholder input on policies related to RPM and RTM. For those concerned with health insurance coverage for chronic disease, this is an ideal moment to voice opinions and concerns.
It will be interesting to observe which aspects of this proposed rule are ultimately solidified, which ones experience revision, and what might be set aside. CMS will be open to receiving comments on the proposed rule until September 11, 2023.
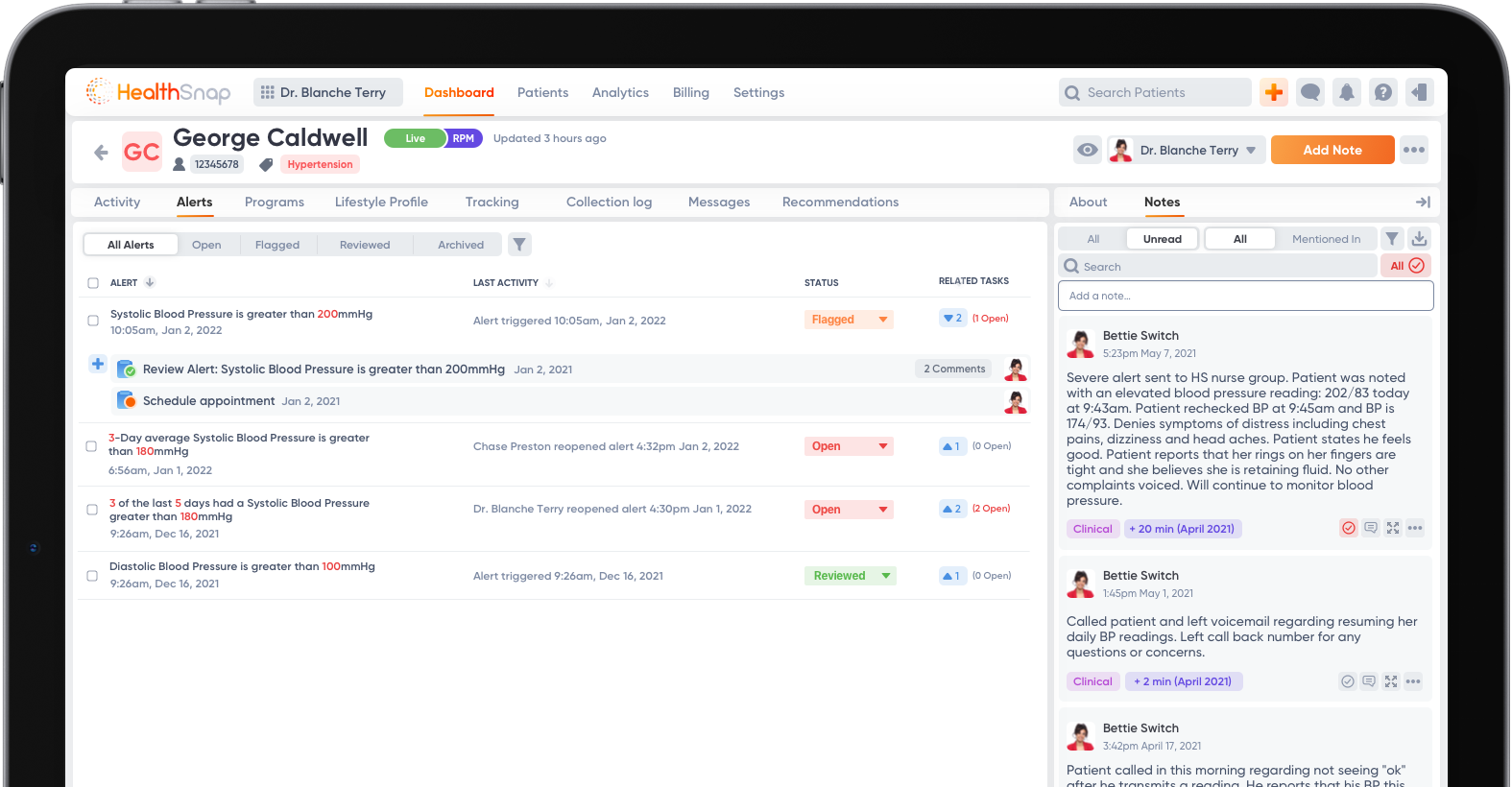
HealthSnap’s Integrated Virtual Care Management Platform
The HealthSnap Virtual Care Platform is strategically designed to assist healthcare organizations and medical professionals in improving the ongoing management of patients’ chronic conditions, while also generating additional revenue streams. With HealthSnap’s virtual care management platform, providers have the opportunity to bill for dedicated resources and CPT codes related to Remote Patient Monitoring (RPM) and Chronic Care Management (CCM).
To learn more about our platform and services or to request a demo, call today at 888-780-1872 (Ext. 3) or click here to schedule a consultation.











