Obesity remains a pressing global health concern. Data from the National Health and Nutrition Examination Survey (NHANES) reveals an alarming fact: over 42% of adults in the United States are classified as obese. Trends indicate that by 2030, half of the US population will struggle with obesity. While new weight loss drugs like Ozempic and Wegovy have shown promise in appetite suppression, they come with potential health risks and the risk of medication dependence.
One effective strategy in obesity management is a holistic focus on whole-person behavioral change. This method has the benefit of long-term sustainability through building new habits. The challenge lies in finding consistent and effective accountability methods for individuals striving to achieve and manage healthy weight and body mass index (BMI), and ultimately, ward off obesity-related health risks.
The Importance of Telehealth in Obesity Management
Telehealth emerges as a powerful solution in the fight against obesity while helping to lower healthcare costs. This digital health approach, designed to manage chronic conditions from the comfort of one’s home, proves invaluable. Through the integration of virtual care management strategies like Chronic Care Management (CCM) and Remote Patient Monitoring (RPM), healthcare providers can deliver:
-
Vital Stats Monitoring: Regular tracking of weight, blood pressure, and other key health metrics to gauge progress and adjust treatment plans accordingly.
-
Behavioral Monitoring: Regular symptom surveys to monitor and address behaviors like addictive eating.
-
Activity Tracking: Utilization of wearable devices to monitor physical activity and encourage a more active lifestyle.
-
Nutrition Coaching and Education: Personalized dietary guidance and nutritional education tailored to individual needs.
As a public health tool, virtual care management combines both behavioral and clinical care, which are pivotal for managing overweight and obesity, helping patients lose weight, and manage chronic conditions, such as high blood pressure, cardiovascular disease, coronary artery disease, and other chronic conditions, at more affordable medical costs.
A Medication-Free Approach to Weight Management
There is a growing emphasis on non-medication solutions in weight management. Numerous digital solutions and applications prioritize behavioral change as a primary means of weight loss. These innovative solutions can serve as the front line of treatment or complement medication-based approaches to sustain weight loss. Digital weight management apps have evolved significantly, with many focusing on holistic health and even boosting self-esteem. Some apps also integrate creative features, such as online community weight challenges, to support users on their weight loss journeys.
Innovators are adopting a personalized approach to weight management. They utilize metabolic testing and glucose monitoring to design individualized treatment plans. Body composition measurements, including body mapping and smart mirrors, are also being incorporated to offer precise care recommendations.

Remote Patient Monitoring companies are at the forefront of this change. They are developing technologies to track weight via smart scales and aggregate data to screen for potential risk factors. These advancements can be effectively integrated with medication-based approaches to stratify appropriate care and monitor patient adherence.
The Role of Remote Patient Monitoring and Chronic Care Management in Obesity Management
Innovative approaches like Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) have emerged as pivotal tools in the ongoing battle against obesity.
Remote Patient Monitoring: RPM is a technology-driven healthcare delivery method that uses cellular devices to collect medical and health-related data from individuals in one location and electronically transmit it to healthcare providers in a different location for ongoing monitoring and assessment.
Chronic Care Management: CCM is a comprehensive care delivery model that involves a systematic approach to managing the healthcare needs of patients with multiple chronic conditions. It aims to improve patient outcomes through better care coordination, regular follow-ups, and patient education.
How RPM Supports Obesity Management
-
Continuous Monitoring of Vital Stats: RPM enables the continuous monitoring of key health metrics like weight, blood pressure, heart rate, and blood glucose levels. For obese patients, regular monitoring of these parameters is vital to track progress, adjust treatment plans, and identify potential health complications.
-
Personalized Care Plans: One of the strengths of RPM is its ability to support personalized care plans matching to individual patient needs. By tracking and analyzing patient data, healthcare providers can design customized dietary and exercise regimens, ensuring a more targeted and effective approach to weight management.
-
Enhanced Patient Engagement: RPM facilitates increased patient engagement and empowerment. Near real-time monitoring and feedback mechanisms encourage patients to actively participate in their care, leading to better adherence to treatment plans and improved health outcomes.
How CCM Supports Obesity Management
-
Comprehensive Care Coordination: CCM provides a structured framework for the effective management of obesity. By coordinating between primary care providers, specialists, and other healthcare professionals, CCM ensures a cohesive and integrated approach to obesity treatment, addressing both medical and behavioral aspects.
-
Regular Follow-ups and Monitoring: Regular follow-ups are a cornerstone of CCM. Through scheduled telehealth visits, healthcare providers can closely monitor patients’ progress, offer timely interventions, and make necessary adjustments to the care plan.
-
Patient Education and Support: CCM emphasizes patient education and support as essential components of obesity management. Through educational resources, counseling, and lifestyle coaching, CCM equips patients with the knowledge and skills needed to make healthier choices, manage their weight effectively, and prevent complications.
The Synergistic Effect of RPM and CCM in Obesity Management

When combined, RPM and CCM offer a synergistic effect in obesity management:
-
Improved Data Accuracy and Timeliness: RPM ensures the continuous and accurate collection of health data, while CCM utilizes this data for better-informed decision-making and treatment adjustments.
-
Enhanced Care Coordination: The seamless integration of RPM and CCM promotes better care coordination among healthcare providers, ensuring a holistic and patient-centered approach to obesity management.
-
Cost-Effective and Efficient Care: By reducing the need for frequent in-person visits and hospital admissions, RPM and CCM contribute to cost savings for both healthcare providers and patients.
RPM and CCM for Nutrition Coaching and Education in Obesity Management
While RPM and CCM are instrumental in monitoring vital health metrics, their potential in nutrition coaching and education is increasingly being recognized as pivotal in obesity management.
-
Near Real-time Feedback and Support: With RPM, patients receive ongoing monitoring of their vitals. This feedback mechanism increases awareness and may empower patients to make healthier food choices, and develop better eating habits, ultimately contributing to weight loss, and improved health outcomes.
-
Comprehensive Nutritional Education: CCM focuses on the importance of patient education as a fundamental component of chronic disease management. Through CCM, healthcare providers can offer comprehensive nutritional education, including information on healthy eating habits, portion control, and meal planning. This educational approach equips patients with the knowledge and skills needed to make informed and healthier dietary choices, promoting sustainable weight loss and preventing obesity-related complications.
-
Personalized Dietary Guidance: Through virtual care management programs, healthcare providers can gain insights into patients’ eating patterns and nutritional intake. This data-driven approach enables support for personalized dietary plans tailored to individual patient needs and preferences, enhancing the effectiveness and adherence to nutritional interventions.
-
Lifestyle Coaching and Behavioral Change: Both RPM and CCM support lifestyle coaching and behavioral change interventions as essential components of obesity management. By addressing the underlying behavioral factors contributing to obesity, RPM and CCM facilitate long-term behavioral change, promoting sustained weight loss and improved overall health.
RPM and CCM for Behavioral Monitoring in Obesity Management
Beyond their traditional roles in monitoring vital health metrics, RPM and CCM play a significant and transformative role in behavioral monitoring, a key aspect of obesity management.
-
Near Real-time Behavioral Tracking: RPM enables the continuous monitoring and tracking of various behavioral parameters crucial in obesity management, including physical activity levels, dietary habits, sleep patterns, and medication adherence. By providing near real-time data and insights into patients’ behaviors, RPM facilitates the early identification of unhealthy behaviors and allows for timely interventions to promote positive behavioral changes.
-
Personalized Behavioral Interventions: Utilizing the data collected through RPM, healthcare providers can design and execute personalized behavioral interventions personalized to individual patient needs and preferences. These interventions may include personalized dietary plans, tailored physical activity recommendations, and behavioral change strategies aimed at promoting healthier lifestyle choices and facilitating weight loss.
-
Behavioral Coaching and Education: Both RPM and CCM support the provision of behavioral coaching and education as essential components of obesity management. Through CCM, healthcare providers can offer comprehensive behavioral education, including information on healthy eating habits, physical activity guidelines, stress management techniques, and strategies to overcome barriers to behavioral change. This educational approach empowers patients with the knowledge, skills, and confidence needed to make and maintain positive behavioral changes, ultimately contributing to improved weight management and overall health.
RPM and CCM for Activity Tracking in Obesity Management
RPM and CCM extend their roles beyond health metric monitoring to encompass comprehensive activity tracking as part of obesity management.
-
Continuous Monitoring of Physical Activity: RPM facilitates near real-time tracking and monitoring of physical activity levels through wearable devices and mobile health applications. These devices collect data on steps taken, distance traveled, calories burned, and active minutes, providing healthcare providers with valuable insights into patients’ daily activity patterns and habits.
-
Personalized Activity Recommendations: Utilizing the data gathered through RPM, healthcare providers can develop and execute personalized physical activity recommendations personalized to individual patient needs, preferences, and capabilities. These recommendations may include specific exercise routines, activity goals, and strategies to increase daily physical activity, aiming to promote a more active lifestyle and facilitate weight loss and management.
-
Activity Coaching and Education: Both RPM and CCM support the provision of activity coaching and education as essential components of obesity management. Through CCM, healthcare providers can offer comprehensive activity education, including information on the benefits of regular physical activity, guidelines for safe and effective exercise, strategies to overcome barriers to physical activity, and motivational support to encourage patients to increase their activity levels and maintain an active lifestyle.
RPM and CCM for Vital Stats Monitoring in Obesity Management

RPM and CCM programs enable the ongoing monitoring of vital health statistics to support obesity management goals. Wearable devices and mobile health apps can monitor metrics such as:
Heart Rate: Monitoring for Cardiovascular Health and Fitness Levels
Heart Rate (HR) refers to the number of times the heart beats per minute (bpm) and is a vital indicator of cardiovascular health and fitness levels. Monitoring heart rate can offer valuable insights into the following:
Resting Heart Rate (RHR)
-
Significance: A higher resting heart rate can be an indicator of lower cardiovascular fitness and increased cardiovascular risk.
-
Monitoring with RPM: RPM allows for continuous monitoring of RHR, providing healthcare providers with valuable insights into the patient’s cardiovascular health and fitness levels over time.
Heart Rate Variability (HRV)
-
Significance: HRV refers to the variation in time between consecutive heartbeats and is an indicator of the autonomic nervous system’s regulation of the heart.
-
Monitoring with RPM: RPM facilitates the tracking of HRV, which can be used to assess stress levels, recovery status, and overall cardiovascular health.
Exercise-induced Heart Rate Response
-
Significance: Monitoring heart rate during physical activities can help assess exercise tolerance, cardiovascular fitness, and the effectiveness of exercise interventions in obesity management.
-
Monitoring with RPM: Wearable devices integrated with RPM technology can monitor heart rate during various activities, providing real-time data on exercise-induced heart rate responses and facilitating the optimization of exercise prescriptions tailored to the patient’s fitness levels and goals.
Blood Pressure: Continuous Tracking for Hypertension Management
Blood Pressure (BP) is the force exerted by the blood against the walls of the arteries as the heart pumps blood throughout the body. Continuous tracking of blood pressure is helpful in managing hypertension, a common comorbidity associated with obesity.
Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP)
-
Significance: SBP represents the pressure in the arteries when the heart beats, while DBP represents the pressure in the arteries when the heart rests between beats. Elevated SBP and DBP levels are indicators of hypertension and increased cardiovascular risk.
-
Monitoring with RPM: RPM enables the continuous tracking of SBP and DBP, facilitating timely interventions to manage and prevent hypertension complications.
Blood Pressure Variability (BPV)
-
Significance: BPV refers to the fluctuations in blood pressure values over time and is an important predictor of cardiovascular events and target organ damage.
-
Monitoring with RPM: RPM allows for the assessment of BPV, providing insights into the stability of blood pressure control and guiding the adjustment of anti-hypertensive medications and lifestyle modifications to optimize blood pressure management.
Oxygen Saturation: Monitoring for Respiratory Function and Overall Health Status
Oxygen Saturation (SpO2) represents the percentage of hemoglobin in the blood that is saturated with oxygen and is a critical indicator of respiratory function and overall health status.
Normal Oxygen Saturation Levels
-
Significance: Normal SpO2 levels range from 95% to 100%. Reduced SpO2 levels indicate hypoxemia, a condition characterized by low oxygen levels in the blood, which can be associated with respiratory and cardiovascular diseases.
-
Monitoring with RPM: RPM enables the continuous monitoring of SpO2 levels, facilitating the early detection of potential respiratory issues and guiding interventions to optimize respiratory function and overall health.
Pulse Oximetry and Respiratory Function Assessment
-
Significance: Pulse oximetry, a non-invasive method used to monitor SpO2 levels, provides valuable information on respiratory function and the efficiency of oxygen delivery to tissues.
-
Monitoring with RPM: RPM utilizes wearable pulse oximeters to monitor SpO2 levels, offering insights into respiratory function and guiding interventions to improve oxygenation and overall health.
How HealthSnap’s Cellular Scale Works for Obesity Management
HealthSnap’s cellular-enabled scale is a groundbreaking RPM device designed to transform the way patients and healthcare providers approach weight management.
Automatic Data Capture
HealthSnap’s cellular scale is engineered for simplicity and user-friendliness. Patients can effortlessly step onto the scale, which then automatically captures and records their weight. This eliminates the need for patients to manually log or input their weight readings, reducing the chances of human error and ensuring precise data collection.
Instant Data Transmission
After capturing the weight data, HealthSnap’s cellular scale utilizes built-in cellular technology to transmit this information directly to the HealthSnap platform in real-time. This immediate data transmission is crucial for continuous monitoring of weight fluctuations, allowing healthcare providers to track and analyze patient progress consistently.
Secure and Efficient Communication
The cellular-enabled feature of the scale ensures secure and efficient communication between the device and the HealthSnap platform. This direct and instantaneous data transfer eliminates the dependence on Wi-Fi or Bluetooth connections, making the process more reliable and reducing potential connectivity issues. The secure data transmission also ensures patient confidentiality and privacy, adhering to healthcare data protection regulations.
Enhanced Data Accuracy and Reliability
The automated and direct data transmission process of HealthSnap’s cellular scale enhances the accuracy and reliability of the weight data collected. By eliminating manual data entry and the potential for transcription errors, the scale provides healthcare providers with dependable and consistent weight measurements. This accurate data is crucial for assessing the effectiveness of obesity management plans and making informed decisions regarding patient care.
Pattern Recognition and Treatment Adjustment
Pattern Recognition: Pattern recognition is a fundamental component of HealthSnap’s RPM and CCM programs for obesity management. It involves the use of advanced algorithms and analytics to identify and analyze patterns, trends, and anomalies in patient health data, particularly focusing on weight fluctuations and related vital signs such as heart rate, blood pressure, and oxygen saturation levels.
Treatment Adjustment: Treatment adjustment in HealthSnap’s RPM & CCM programs involves making timely and informed modifications to the patient’s obesity management plan based on the insights gained from the pattern recognition process. This proactive approach ensures that the treatment plan is continuously optimized to meet the patient’s evolving health needs, ultimately enhancing the effectiveness of the obesity management strategy.
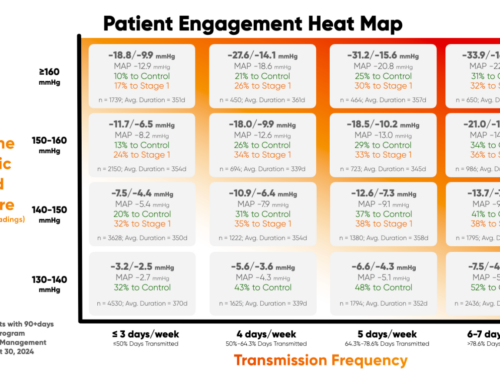
How HealthSnap’s RPM and CCM Programs are Helping Healthcare Providers Achieve the Goals in Obesity Management
HealthSnap’s innovative RPM and CCM programs are at the forefront of virtual care management, providing comprehensive solutions to healthcare providers.
Continuous Weight Monitoring with Cellular Scale
HealthSnap’s cellular scale enables patients to measure their daily body weight accurately. The data is then seamlessly transmitted to healthcare practitioners, allowing them to actively monitor patients between in-person visits. This real-time weight tracking plays a crucial role in tailoring obesity management plans to individual patient needs. By identifying patterns and assessing the effectiveness of the treatment plans, healthcare providers can offer timely interventions and adjustments, optimizing patient outcomes.
Remote Monitoring and Identification of Lifestyle Interventions
In addition to the cellular scale, HealthSnap’s RPM and CCM platform and alerts support potential lifestyle interventions that may otherwise go unnoticed during clinical visits. This comprehensive approach to virtual care management creates an environment for patients to discuss and address weight management issues.
Outcomes and Patient Satisfaction
HealthSnap’s RPM programs have demonstrated promising outcomes in obesity management. According to outcomes data, patients enrolled in HealthSnap’s RPM programs experienced an average weight loss of 5 lbs. Furthermore, an overwhelming eighty-four percent of patients reported a greater sense of control over their health. The consistent monitoring and feedback from care providers enhanced the patients’ understanding of their health, with 70 percent of patients showing improved health outcomes.
Proactive and Successful Weight Management with HealthSnap
HealthSnap offers a comprehensive RPM solution for obesity management programs, equipped with cellular-enabled connected devices, AI assistance, and population analytics. The integrated Virtual Care Management Platform caters to multi-specialty medical practices and healthcare providers alike, offering an all-in-one solution for effective and personalized obesity management.
Schedule a Demo Today
HealthSnap’s RPM and CCM programs are revolutionizing obesity management by offering a proactive and personalized approach to patient care. With promising outcomes and high patient satisfaction rates, HealthSnap is the ideal choice for healthcare providers aiming to enhance their chronic condition management strategies.
To learn more about virtual care management solutions for obesity management and to discover how HealthSnap can benefit your healthcare organization, please schedule a demo with one of our specialists by calling 888-780-1872 or contact us online.