The healthcare landscape is rapidly evolving, and with the advancements in technology, there has been a significant shift toward patient-centric care. Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) programs have emerged as powerful tools to enhance patient care and improve outcomes. Integrating these programs with Electronic Health Records (EHR) can further streamline care coordination, improve data accuracy, and enhance the overall patient experience. In this guide, we will explore the key steps and considerations involved in building a scalable Remote Patient Monitoring and CCM program with EHR integration.
Understanding Remote Patient Monitoring and Chronic Care Management
Remote Patient Monitoring (RPM)
Remote Patient Monitoring involves the use of connected devices to collect and transmit patient health data to healthcare providers. These devices can monitor vital signs, such as blood pressure monitors for blood pressure, to track symptoms and provide real-time data for patient interventions. RPM enables continuous monitoring of patients outside of traditional healthcare settings, allowing for early detection of health issues and timely intervention.
Chronic Care Management (CCM)
Chronic Care Management focuses on the comprehensive management of patients with chronic conditions. It involves care coordination, medication management, patient education, and regular follow-ups. CCM aims to improve patient outcomes, reduce hospital admissions, and enhance the overall quality of life for individuals living with chronic illnesses.
Benefits of EHR Integration with RPM and CCM Programs
Electronic Health Record (EHR) technology has revolutionized the healthcare industry by digitizing patient health information. EHR systems enable healthcare providers to capture, store, and access patient data securely. They provide a comprehensive view of a patient’s medical history, diagnoses, treatments, medications, and other relevant personal health information throughout. Leveraging EHR data is essential for effective Remote Patient Monitoring and CCM programs as it allows healthcare providers to monitor patients, track progress, and make data-driven decisions. Here are the key benefits of EHR integration with RPM and CCM programs:
Streamlined Data Management
Integrating RPM and CCM programs with EHR systems eliminates the need for manual data entry and ensures accurate and up-to-date patient information. Real-time data from remote monitoring devices can be seamlessly transmitted to the EHR, providing a comprehensive view of the patient’s health status and enabling healthcare providers to make informed decisions.
Enhanced Care Coordination
EHR integration enables seamless communication and collaboration among healthcare providers involved in the patient’s care. Care plans, medication lists, and treatment guidelines can be shared and updated in real time, ensuring consistent and coordinated care across different healthcare settings.
Improved Patient Engagement
EHR integration facilitates patient engagement by enabling patients to access their health information, review test results, and communicate with their healthcare team. Empowering patients with access to their data promotes active participation in their care and fosters a sense of ownership and responsibility.
Data Analytics and Population Health Management
Integrating Remote Patient Monitoring and CCM programs with EHR systems provides a wealth of data that can be leveraged for population health management initiatives. Analyzing aggregated data from multiple patients can help identify trends, risk factors, and opportunities for proactive interventions to improve overall population health.
Key Steps to Building a Scalable RPM and CCM Program with an EHR Integration
Identify Program Goals and Objectives
Clearly define the goals and objectives of the RPM and CCM program. Determine the target patient population, the specific chronic conditions to be managed, and the desired outcomes. Aligning program goals with a health systems priorities, for example, is crucial for successful implementation.
Select a Reliable EHR System
Choose an electronic health information system that supports seamless integration and promotes interoperability with RPM and CCM platforms. Ensure that the EHR vendor has experience in interoperability and adheres to industry standards. Evaluate the system’s scalability, security measures, and user-friendliness to meet the needs of your organization.
Assess Workflow and Process Changes
Evaluate existing workflows and identify areas that need modification to accommodate RPM and CCM activities. Determine how remote physiologic monitoring services data will flow into the EHR, who will be responsible for monitoring and analyzing the data, and how care coordination will be facilitated. Engage all stakeholders, including physicians, nurses, and administrative staff, to ensure smooth implementation.
Choose RPM and CCM Technology Solutions
Select RPM and CCM technology solutions that align with your program goals and integrate seamlessly with your chosen EHR system. Consider factors such as medical device, compatibility, ease of use for patients, data security measures, and data transmission capabilities. Work closely with the technology vendors to customize the solutions based on your specific requirements.
Establish Patient Data Governance Policies
Develop comprehensive data governance policies to ensure the security, privacy, and integrity of patient data. Define who has access to the data, how it will be protected, and how data breaches will be handled. Comply with relevant regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), to maintain patient safety and confidentiality when it comes to Protected Health Information (PHI).
Train Staff and Educate Patients
Provide thorough training to healthcare staff on the proper use of RPM and CCM technologies and the integration digital health tools with the EHR system. Educate patients on the benefits of remote monitoring and chronic care management, and provide clear instructions on how to use the devices and engage with the program. Continuous support and education are vital for successful adoption.
Monitor and Evaluate Program Performance
Establish metrics to assess the program’s performance and regularly monitor key indicators. Evaluate patient outcomes, healthcare utilization, patient satisfaction, and staff productivity. Analyze the data collected from RPM and CCM platforms to identify areas for improvement and optimize the program’s effectiveness.

Overcoming Challenges and Ensuring Success of Virtual Care Programs
Technical Challenges
Address the technical infrastructure challenges such as data integration, interoperability, and system compatibility early in the planning phase. Collaborate with IT experts and EHR vendors to ensure a seamless and secure data flow (health data interoperability) between RPM, CCM, and EHR systems.
Regulatory and Compliance Considerations
Stay up-to-date with relevant regulations and compliance requirements, such as HIPAA and data protection laws. Implement strict data security measures, including encryption and access controls, to protect patient information and comply with privacy regulations.
Patient Engagement and Adoption
Implement strategies to encourage patient engagement and adoption of RPM and CCM programs. Provide clear communication, educational resources, and ongoing support to patients. Address any concerns or barriers to participation to ensure active patient involvement.
Collaboration and Communication
Foster collaboration and effective communication among all stakeholders involved in the RPM and CCM program. Encourage open dialogue, share best practices, and address any challenges or bottlenecks that arise during implementation. Regularly review and refine processes to optimize care delivery.
Building a scalable RPM and CCM program with EHR integration is a complex but rewarding endeavor. By leveraging the power of technology and integrating RPM and CCM programs with EHR systems, healthcare organizations can enhance care coordination, improve patient outcomes, and optimize resource utilization. It is essential to carefully plan and execute each step, engage all stakeholders, and continuously monitor and evaluate the program to ensure long-term success in delivering patient-centered care.
Integration into the EHR is Pivotal for Scalable RPM Program Deployments in a Health System
Effective integration into health system Electronic Health Record (EHR) systems is vital for the successful implementation of remote patient monitoring (RPM) programs. While there are many factors that contribute to the success or failure of RPM implementation, EHR integration stands out as the most critical feature for managing and scaling RPM programs effectively.
When RPM services integrate seamlessly with existing EHR systems, it eliminates interruptions and prevents an increase in administrative labor. Without EHR integration, clinical staff would have to navigate between two separate computer systems themselves, leading to reduced efficiency and increased workload. However, with effective EHR integration, the health system can use an easy-to-use platform that automatically works within their familiar EHR system, eliminating the hassle of working with multiple systems.
One of the key advantages of EHR integration is its simplicity, allowing anyone with any technical skill level to use the remote patient monitoring platform. This simplification facilitates faster implementation of RPM programs, reduces staff training costs, and enhances automation, ultimately reducing the workload for clinics and providers.
As RPM programs generate a higher volume of patient touchpoints, data, and reports, it becomes essential to reflect all this information in the clinic’s existing medical record system. EHR integration enables seamless deployment and management of RPM programs while ensuring that all relevant data is captured and stored within the EHR system.
In addition, EHR integration enables more effective scalability. By eliminating the need to work with two separate systems, clinics can expand their remote service provision and take on more patients without burdening their clinical staff with additional labor.
The benefits of EHR integration for health systems extend beyond simplified workflows and scalability. One notable improvement is the ability to digitally sign referrals. With EHR integration, patient referrals can be generated directly from the EHR system, seamlessly flowing into the service provider processes. This streamlines patient onboarding and allows for a smooth transition from in-person visits to referrals for telemonitoring services with a simple press of a button in the EHR.
EHR integration also enables better tracking of measurable data in remote monitoring care, improving the quality of value-based care and enhancing reporting and communication of risk scoring and clinical results between insurance providers and clinics.
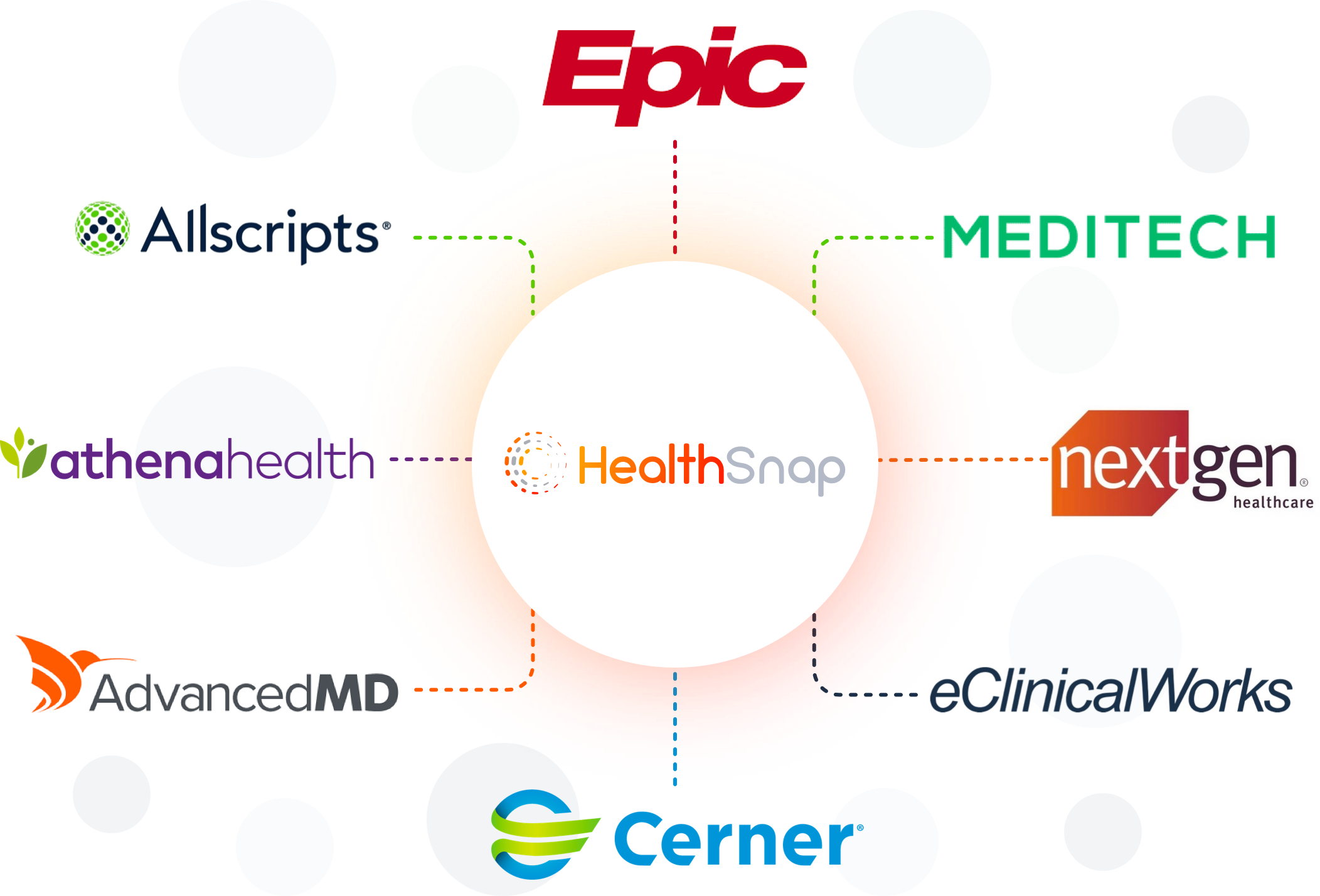
When choosing an RPM service provider, it is prudent to select one that offers robust EHR integration. Some providers may struggle to offer seamless integration into clinical EHR systems, leading to long-term management issues for RPM programs. On the other hand, effective RPM and CCM program providers like HealthSnap ensure the automatic integration of biometric data and reports from RPM into the EHR. This level of integration makes the provision of remote care easier and more effective for practitioners and clinics, facilitating the successful scaling of RPM programs and revenue improvement.
Therefore, clinics considering a transition to virtual care should prioritize EHR integration when selecting an RPM service provider. It is essential to ensure that the chosen provider offers seamless integration with the clinic’s EHR system, as it significantly contributes to the success of RPM implementation and long-term management.
HealthSnap: Empowering Healthcare Providers with an EHR-Integrated Virtual Care Management Platform
HealthSnap is an innovative health technology company that offers a comprehensive platform to empower healthcare organizations in building scalable RPM and CCM programs with EHR integration. HealthSnap’s standard EHR integration package provides a healthcare organization with the convenience to work out of their existing EHR while harnessing the benefits of working with HealthSnap to reduce the cost of care and improve outcomes with Remote Patient Monitoring.
The objective of EHR integration is to maximize convenience while eliminating the additional time spent logging into and navigating multiple systems, including manual and double entry of information.
HealthSnap: The Catalyst in RPM and CCM Integration with EHR
Let’s explore some key features and benefits of HealthSnap’s virtual care platform:
Seamless EHR Integration
HealthSnap’s platform seamlessly integrates with leading EHR systems, ensuring a smooth flow of patient data. This integration eliminates the need for manual data entry, reduces administrative burden, and enhances data accuracy. Healthcare providers can access real-time patient information directly from the EHR, enabling timely interventions and personalized care plans.
Patient Data Collection
HealthSnap’s platform enables healthcare organizations to collect patient data through various means, such as connected devices, mobile apps, and patient-reported outcomes. This data includes vital signs, symptoms, medication adherence, and lifestyle factors. The platform ensures secure data transmission and storage, adhering to strict privacy and security regulations.
Data Analytics and Insights
HealthSnap’s robust analytics engine transforms raw patient data into actionable insights. Healthcare providers can visualize trends, identify anomalies, and gain a comprehensive understanding of patient’s health status. These insights help in risk stratification, early intervention, and personalized care planning, leading to improved patient outcomes.
Care Coordination and Communication
HealthSnap’s platform facilitates seamless communication and collaboration among care teams. Healthcare providers can securely share patient information, exchange messages, and coordinate care plans. This streamlined communication enhances care coordination, reduces medical errors, and ensures continuity of care across different healthcare settings.
Patient Engagement and Education
HealthSnap’s patient-facing features empower individuals to actively participate in their own care. Patients can access their health data, view personalized care plans, set health goals, and receive educational materials. The platform promotes patient engagement, self-management, and adherence to treatment plans, ultimately leading to better health outcomes.
Scalability and Customization
HealthSnap’s platform is designed to scale according to the needs of healthcare organizations. Whether it’s a small clinic or a large hospital network, the platform can adapt to the organization’s requirements. Additionally, HealthSnap offers customization options to align with existing workflows and clinical protocols, ensuring seamless integration into the healthcare ecosystem.
HealthSnap’s platform plays a crucial role in helping healthcare organizations build scalable Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) programs with EHR integration. By seamlessly integrating with EHR systems, HealthSnap empowers healthcare providers to collect patient data, gain actionable insights, coordinate care, and engage patients effectively.
This comprehensive approach enhances patient outcomes, improves care coordination, and reduces healthcare costs. As the healthcare industry, especially Medicare services, continue to embrace patient-centric care models, HealthSnap’s innovative platform serves as a catalyst in transforming healthcare delivery and elevating the standard of patient care.
A Review of Other Leading EHR Solution Providers
AthenaHealth
AthenaHealth’s EHR solution enables healthcare providers to focus on delivering care, prioritizing the patient experience and efficient workflows. By utilizing their cloud-based EHR, providers can stay ahead of industry changes while streamlining documentation and ensuring exceptional care delivery.
The EHR’s documentation features are designed to enhance encounter workflow, reduce administrative tasks, and provide complete patient information. By utilizing intuitive workflows, customizable templates, macros, and accelerators, documentation becomes easier and more efficient. Additional features like Pre-Encounter Prep and Focused Encounter further optimize documentation time.
To cater to different specialties, AthenaHealth’s EHR offers specialty-specific workflows, allowing clinicians to tailor the documentation process to their specific needs. The EHR also supports mobile documentation through the athenaOne app, enabling physicians to document encounters without returning to a computer.
Real-time patient insights are accessible through the EHR, providing clinicians with up-to-date patient data and insights from AthenaHealth’s network, seamlessly integrated into their standard workflows.
The EHR system ensures patient information is easily accessible within the patient’s record, minimizing the time clinicians spend searching for crucial data. By automatically incorporating data from across the healthcare ecosystem, including comprehensive networks like CommonWell and Carequality, the EHR provides a comprehensive view of a patient’s care history.
Improved care coordination is facilitated through collaboration features embedded within the patient chart, allowing clinicians to work together on patient care plans in real time.
AthenaHealth acknowledges the challenges posed by industry changes such as evolving reimbursement models, value-based care, and regulatory requirements. By continuously tracking changes and ensuring compliance, AthenaHealth’s EHR alleviates the burden on clinicians, allowing them to focus on providing quality patient care.
Identifying and addressing potential gaps in care is made easier with the EHR’s accurate and actionable insights that surface directly within the clinical workflow, enabling providers to close care gaps and enhance value-based care results. Additionally, the EHR’s flexible technology and quality performance team assist healthcare providers in meeting regulatory requirements and optimizing their quality performance.
In addition to the core EHR capabilities, AthenaHealth offers expanded services that enhance daily workflows and enable extraordinary care delivery. These services include Voice Powered Services for improved clinical efficiency, Population Health Support for coordinating care and managing patient populations, and Telehealth services for convenient and essential care delivery.
NextGen
NextGen’s award-winning EHR system is highly reliable and trusted by healthcare providers. Designed to improve work-life balance, provide easy access to data, and deliver positive clinical and financial outcomes, NextGen’s integrated healthcare solutions aim to enhance the healthcare experience for all stakeholders.
The integrated platform increases productivity, improves financial outcomes, simplifies information exchange, and enhances the patient experience.
NextGen focuses on empowering clinicians by streamlining and customizing workflows, promoting care team collaboration, enabling mobile documentation for increased face time with patients, and ensuring compliance with regulatory requirements.
Patient engagement is enhanced through improved patient engagement tools, reducing staff time spent on administrative tasks, offering telehealth capabilities for convenient care, and enabling direct connections with patients.
The population health feature enables healthcare providers to target higher-risk patients, close gaps in care, and identify patients who may impact outcomes. Seamless communication and care coordination are supported within the platform, along with the identification of fee-for-service revenue opportunities.
NextGen offers specialized solutions tailored to various medical specialties, including ambulatory surgical centers, behavioral health, cardiology, community health, internal medicine, multi-specialty practices, ophthalmology, optometry, orthopedics, pediatrics, physical therapy, podiatry, primary care for small practices, and urgent care.
NextGen Office is an all-in-one solution designed for small practices, providing a cloud-based EHR, practice management platform, and a patient portal to streamline operations and focus on care.
NextGen Enterprise caters to mid-size and enterprise practices, offering a scalable and adaptable EHR solution that can be customized according to specialty, workflow, and preferences. This comprehensive solution includes specialty-specific clinical content, best-in-class practice management, advanced analytics, revenue cycle management, a clearinghouse, patient engagement tools, and mobile documentation capabilities.
By utilizing NextGen’s integrated system, healthcare providers benefit from seamless EHR, practice management, interoperability, and patient access, self-scheduling, virtual visits, check-in, examination, documentation, check-out, billing, and other features.
NextGen’s EHR system provides clinical templates for 26 specialties, offering pre-built content and reporting capabilities to improve productivity and outcomes. Providers can customize these templates as needed. NextGen prioritizes patient experience by providing a user-friendly patient portal for communication, appointment scheduling, access to medical records, form completion, and online bill payment.
Community care management is facilitated through NextGen’s population health solution, which syncs with the EHR, provides risk stratification for patient populations, identifies care gaps, and supports patient outreach. The availability of a mobile extension of the practice allows providers to work efficiently from anywhere, with all documentation seamlessly flowing into the patient chart.
NextGen emphasizes the importance of data accessibility, enabling secure health information exchange and integration across various health information systems. Interoperability, speed, security, cost-effectiveness, and compliance are key aspects of their healthcare data exchange capabilities.
For efficient IT management, NextGen offers secure hosting services through Amazon Web Services (AWS), reducing the burden on healthcare organizations and ensuring scalability, simplified upgrades, and cost reduction.
Epic
Epic is a reputable and widely-used electronic health record (EHR) system provider, known for its long-standing presence in the industry since its establishment in 1979. With over 250 million patients having current electronic records in their software, Epic has established itself as a trusted and experienced EHR provider.
The Epic EHR platform offers a comprehensive set of features for telehealth, billing, scheduling, reporting, and e-prescriptions. It seamlessly integrates with external pharmacies, facilitating efficient communication of e-prescriptions. For a detailed understanding of Epic EHR’s features, pricing, and pros and cons, readers can refer to a comprehensive review available.
Epic EHR serves as a solution to improve patient engagement, automate revenue and coding, manage health insurance operations, and gain predictive insights. The fees for Epic EHR vary depending on the organization’s size, and interested providers can contact sales representatives for a customized quote.
Interoperability is a key aspect of Epic EHR, allowing providers to share patient records both within the Epic community and with providers using other EHR systems. With a focus on secure data exchange, Epic facilitates the data sharing up of to 100 million records per month.
The platform includes a patient portal that enables patients to communicate with their doctors, schedule appointments, complete questionnaires, and access their health information. In-patients can utilize the MyChart Bedside feature to communicate with their care team and view their schedule.
Epic EHR streamlines claims and billing management, automating the claims processing workflow and providing visibility into patient eligibility and insurance operations.
While Epic EHR offers a feature-rich solution, the cost of health plans itself can increase significantly with additional features and capabilities. Large healthcare organizations may find the solutions affordable, but smaller practices may prefer to focus on essential features that align with their budget.
Ensuring interoperability is essential for healthcare providers utilizing Epic. Epic HER enables the seamless sharing of 100 million records per month within the Epic community and with providers using different electronic health record systems. Regardless of whether your organization utilizes a different EHR system or doesn’t have an EHR at all, there are multiple avenues available to access and exchange patient records within the Epic community.
In summary, AthenaHealth, NextGen, and Epic offer robust EHR solutions with various features and capabilities to enhance healthcare delivery and improve patient outcomes. Each provider caters to different needs and sizes of healthcare organizations, offering specialized functionalities and customization options to meet the unique requirements of healthcare providers across specialties and practice sizes.
The Role of Electronic Health Records (EHR) in RPM and CCM
Healthcare professionals widely recognize the advantages of Remote Patient Monitoring (RPM), including the reduction of readmissions and cost savings. However, challenges may arise when implementing an RPM program in a healthcare organization. Clinicians and care teams may be hesitant to take on additional responsibilities amidst their already heavy workload, and administrators may have concerns about the program’s revenue generation.
The solution to these issues is straightforward: integrating the workflow of the RPM program into the Electronic Medical Record (EHR) system. By doing so, the burden on healthcare teams is lessened, as it becomes simpler to document a patient’s health record and treatment and facilitate billing. Moreover, this integration enhances clinician acceptance, as all workflow and administrative processes are seamlessly managed within a system they are already familiar with.
HealthSnap: Your Trusted Virtual Care Management Platform

HealthSnap is the ultimate solution that revolutionizes virtual care management for chronic conditions. We offer a comprehensive operating system with seamless EHR integration, uniting the entire care team to achieve optimal performance and enhance patient outcomes. With our cutting-edge virtual care management platform, we facilitate the shift from reactive, episodic care to proactive, continuous care that extends into the patient’s home for health systems and healthcare providers.
Through near real-time data transmissions, HealthSnap enables closer and more personalized engagement between healthcare providers and patients. This not only fosters stronger relationships but also empowers data-driven decision-making for effective care management. If you’re seeking to consolidate all your virtual chronic care delivery needs onto a single platform, HealthSnap is the ideal choice.
Contact us at 888-780-1872 or click here to set up a meeting and we will be happy to respond to your questions and provide a product demonstration.










