By Wesley Smith, Ph.D., HealthSnap Co-Founder & Chief Scientific Officer
As we progress deeper into the digital era, the healthcare landscape is undergoing a significant transformation. A shining beacon in this evolution is the rise of remote patient monitoring (RPM) and chronic care management (CCM) programs. These groundbreaking initiatives have the potential to significantly improve the Merit-based Incentive Payment System (MIPS) scores for healthcare providers.
The Intersection of Remote Patient Monitoring, Chronic Care Management, and Merit-Based Incentive Payment System
The MIPS program, devised by the Centers for Medicare & Medicaid Services (CMS), assesses healthcare providers based on four key performance categories: Quality, Cost, Improvement Activities, and Promoting Interoperability. The overarching objective is to enhance healthcare quality, curtail costs, and optimize health outcomes as we’ve seen at HealthSnap.
RPM and CCM can contribute positively to all these areas, leading to improved MIPS scores. Here’s how:
Enhancing Quality of Care through RPM and CCM
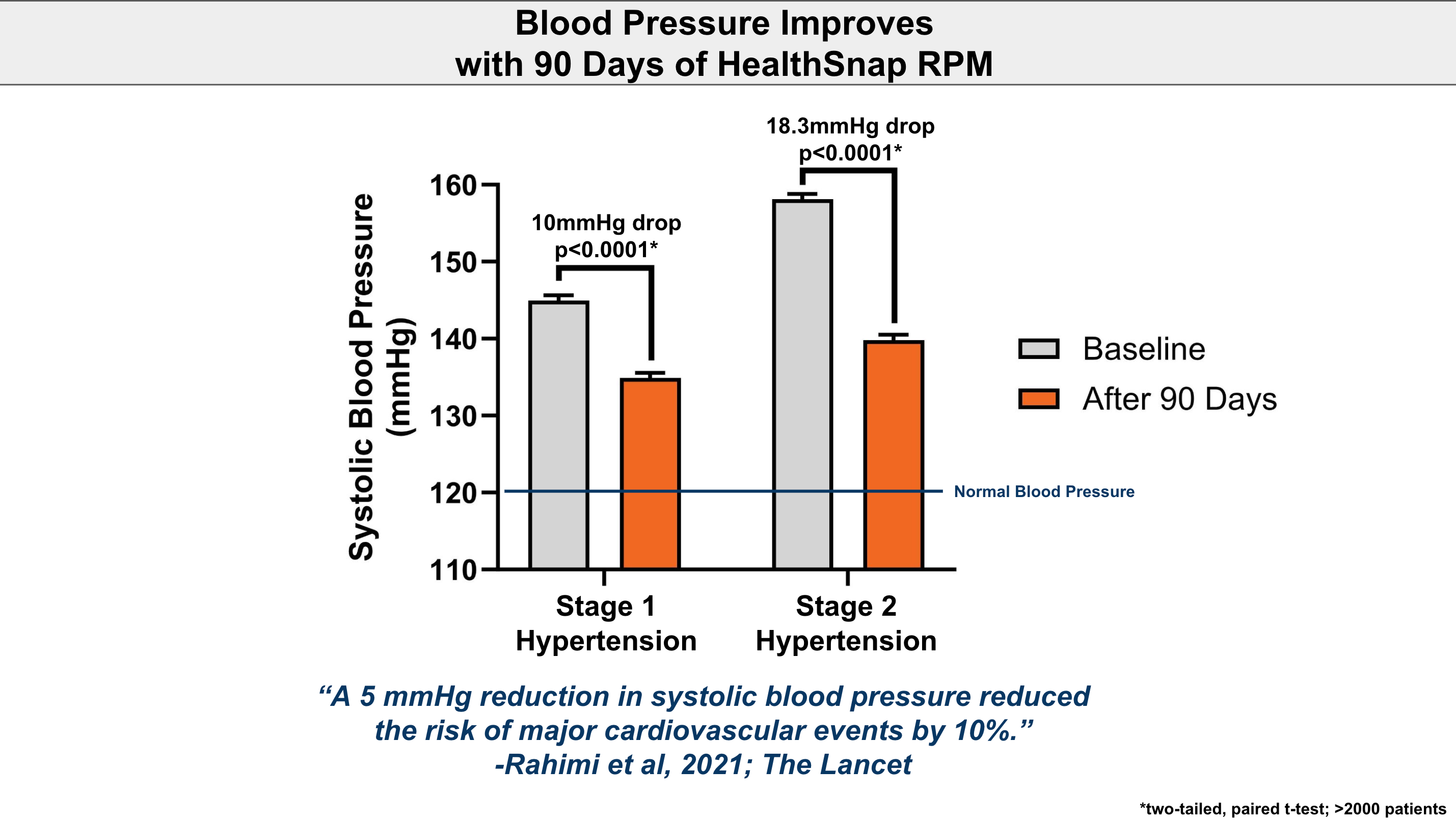
RPM enables healthcare providers to monitor patients’ health data remotely in real time. It allows for timely interventions based on the insights gathered. Similarly, CCM programs ensure that patients with chronic conditions receive consistent, coordinated care. This proactive approach can significantly enhance patient outcomes, reflecting positively on the ‘Quality’ category of MIPS.
Reducing Costs with Effective Management
Effective management of chronic conditions through Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) can lead to fewer hospitalizations and readmissions, thereby reducing healthcare costs. By diminishing the need for in-person visits, these programs also decrease associated costs. This cost-effectiveness aligns with the ‘Cost’ category of MIPS, potentially boosting scores in this area.
Fostering Improvement Activities with Innovation
The Improvement Activities category, formerly known as Clinical Practice Improvement Activities (CPIAs), is a key component of the MIPS. This category measures a clinician or group’s engagement in activities that enhance clinical practice. It emphasizes actions aimed at improving patient safety, care coordination, beneficiary engagement, and population health management.
Examples of these activities may include shared decision-making, regular use of patient safety practices, or participating in initiatives promoting the use of patient-reported outcome measures. Clinicians must attest to engaging in specific activities for a minimum of 90 days during the performance period to earn credit in this category, which accounts for 15% of the total MIPS score.
In this context, RPM and CCM programs can play a pivotal role in contributing to Improvement Activities. By implementing RPM and CCM, healthcare providers can enhance clinical practice and patient safety, both of which are integral to the Improvement Activities category.
These programs are prime examples of innovative technologies that facilitate real-time monitoring of patient’s health data and ensure consistent, coordinated care for patients with chronic conditions. Therefore, they perfectly align with the aims of the Improvement Activities category, which encourages innovation and the adoption of new practices to improve patient care.

Promoting Interoperability with Technology
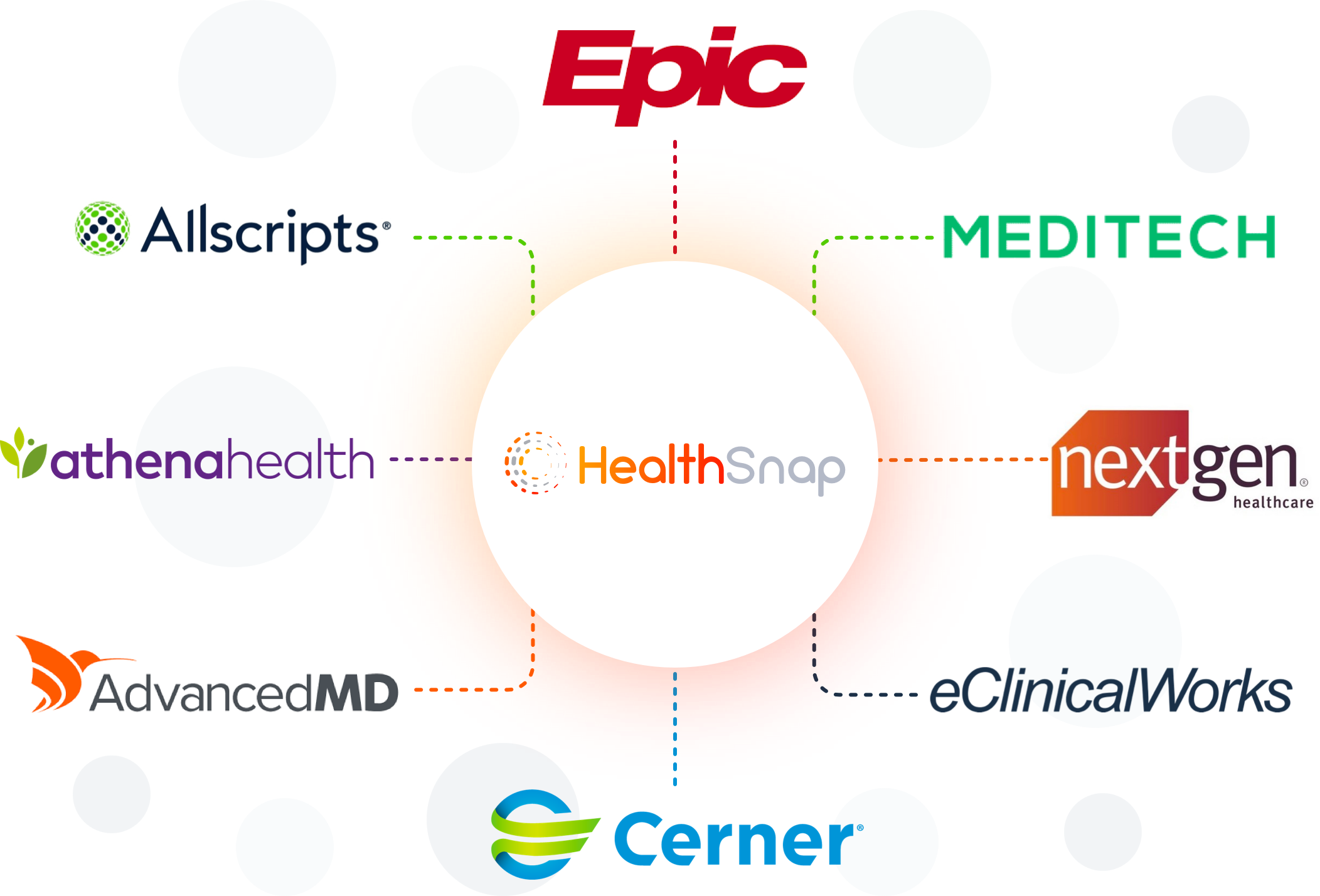
Within the framework of the MIPS, Promoting Interoperability is a significant category that emphasizes the use of certified electronic health record (EHR) technology to improve patient access to their health information and facilitate the seamless exchange of information between providers.
CCM Care Navigators can contribute significantly to this category. Their role involves diving into a participating patient’s EHR to coordinate care, track patient health data, and communicate crucial information to other healthcare providers. Here’s how:
-
Enhanced Patient Access: Care Navigators can help patients navigate their EHRs, enabling them to understand their health data, manage their conditions better, and make informed decisions about their health.
-
Improved Information Exchange: Care Navigators utilize EHRs to share information with other healthcare providers. This interoperability facilitates coordinated care, especially for patients with chronic conditions who often see multiple providers.
-
Patient Engagement: By using EHRs, Care Navigators can engage patients in their care. They can send reminders for appointments or medications, share educational resources, and respond to patient queries. This active engagement can lead to better health outcomes and patient satisfaction.
-
Data Analysis for Quality Improvement: Care Navigators can analyze data from EHRs to track a patient’s progress, identify areas for improvement, and implement changes to enhance care quality.
-
Health Information Exchange (HIE): Care Navigators, through the use of EHRs, can participate in HIEs. This not only improves the continuity of care but also contributes to public health reporting and population health management, key aspects of Promoting Interoperability.
By performing these roles effectively, CCM Care Navigators can contribute to the ‘Promoting Interoperability’ category of MIPS, enhancing not just the MIPS scores for healthcare providers but also leading to improved patient care and outcomes.
Addressing Gaps in MIPS Measures with RPM and CCM
However, a study published in the Annals of Family Medicine highlighted potential disparities in the MIPS measures. The research found gaps in the MIPS measures that could exacerbate healthcare inequities for marginalized populations, specifically related to patient access, experience, and interpersonal care.
The American Academy of Family Physicians (AAFP) has also raised concerns about these gaps and urged the CMS to address them. The researchers concluded that policymakers should broaden the spectrum of MIPS quality measures to include areas such as quality and equity. This could help reduce disparities between patient populations and improve overall care and health outcomes. If these gaps remain unaddressed, healthcare inequities could become more pronounced.
This is where RPM and CCM can play a significant role. By improving access to healthcare delivery for marginalized populations, RPM can mitigate this potentially negative impact of MIPS measures. The combination of RPM with MIPS participation can create a synergistic effect, enhancing access to care for marginalized populations, and improving healthcare outcomes overall.

Conclusion: A Win-Win Solution
The potential of RPM and CCM in improving MIPS scores is certainly promising. However, successful implementation hinges on several factors, including the choice of the right technology, ensuring patient engagement, and selecting the appropriate measures for reporting in each MIPS category.
The incorporation of such technologies can be seen as using technology for the greater good, especially in U.S. healthcare, where there have been persistent gaps in efficiency. Often, a dichotomy exists between revenue-generating healthcare measures and those that benefit the patient, who should always be at the heart of every healthcare equation. By prioritizing patient-centric measures like RPM and CCM, we can begin to bridge this gap, ensuring that care delivery aligns with both the needs of the patient and the objectives of the healthcare system.
As healthcare continues to evolve, leveraging RPM and CCM programs could pave the way for better patient care and improved MIPS scores. This ultimately leads to a win-win situation for healthcare providers and patients alike. As we embrace these advancements, we move closer to a future where quality healthcare is not only accessible and efficient but also patient-focused and equitable. We are making the most of innovative technologies at our disposal, transforming them into tools for enhanced care, improved health outcomes, and the ultimate betterment of the healthcare landscape.











Leave A Comment
You must be logged in to post a comment.