By Wesley Smith, Ph.D., HealthSnap Co-Founder & Chief Scientific Officer
Introduction: Boosting Engagement and Enabling Patients to Take Control of Their Health
A patient-focused care plan is crucial for improved health outcomes, but it requires a solid grasp of the human psyche. In this article, I’ll explore the fascinating link between behavioral change and healthcare, using scientific evidence and insights from my career, which ranges from running a wellness center to working as a geriatric hospital physiologist and researcher. Now, as the co-founder and Chief Scientific Officer of HealthSnap, these experiences helped inform our company’s care navigation strategies in chronic care management and remote patient monitoring.
For effective patient engagement, it’s important to emphasize three fundamental principles related to behavior change – the Yerkes-Dodson inverted U theory, the Fogg Behavior Model, and the Transtheoretical Model. By incorporating these principles into care navigation strategies, we can enhance remote monitoring and chronic care management. This truly patient-centered approach can increase engagement and empower patients to take greater control of their health.
Striking the Balance: Applying the Yerkes-Dodson Law in Patient Care Navigation for Digital Healthcare
Patient engagement is the cornerstone of success in the healthcare industry, and without it, even the most meticulously crafted plans and strategies risk falling flat. It’s not enough to simply center our services around patients; we must aim to become an integral part of their lives. This becomes particularly significant in chronic care management where patient engagement and follow-through on care plans are critical. Here, a care navigator’s understanding of readiness-to-change and human motivation, such as the Yerkes-Dodson inverted U theory, plays a pivotal role. This psychological principle suggests that optimal performance occurs under moderate pressure, offering a valuable framework for engaging patients effectively.
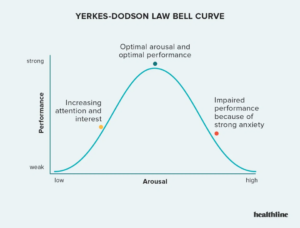
This psychological principle suggests that optimal performance occurs under moderate pressure, offering a valuable framework for engaging patients effectively.
In applying the Yerkes-Dodson law to digital healthcare patient navigation, the challenge is to motivate patients without causing excessive stress. Ideally, education should fuel a patient’s desire for change, providing a clear vision of the improved wellbeing that awaits. If we fail to inspire and sufficiently motivate the patient, it could lead to disinterest and a lack of engagement, causing them to not take their care plan and goals seriously. On the other hand, an overzealous approach with too much coaching or commanding change can lead to stress, discouragement, and potentially patients dropping out. Remote care management services should spark curiosity and inspire participation without overwhelming them with daunting challenges. Sometimes, the ‘less is more’ approach proves to be the winning strategy. The focus should be on striking a balance between establishing a bond with the patient and concentrating on essential tasks to optimize their health and wellbeing.
Interestingly, there is data to suggest that goal setting, while crucial within a patient’s care plan, could occasionally hinder patient engagement. Setting a challenging goal might lead to disappointment if they fall short, or even a sense of defeat if their health measures worsen rather than improve.
The solution lies in striking the right balance. Along with setting goals, there should be a strong emphasis on educating patients about what to expect, how to remain focused on achieving a goal, and understanding that it’s okay if the goal isn’t met this time around. It’s more about the journey than the destination, taken at a pace that suits the individual.
Patient care navigation should be leveraged as an opportunity to motivate, inspire, and empower patients to take charge of their health and quality of life. Patients don’t need a ‘Sage On A Stage’ directing their every move. What they truly need is a ‘Guide on the Side’, assisting them in their journey towards better health with understanding, empathy, and support.
Applying the Fogg Behavior Model to Remote Patient Monitoring and Chronic Care Management
Getting patients to adhere to lifestyle changes can seem like a formidable task, often impeded by two primary obstacles: overly ambitious expectations and a lack of sustained motivation. These challenges become particularly pronounced when managing chronic care remotely. However, through emphasizing education, setting achievable goals, and cultivating a supportive environment, we, as healthcare professionals, can effectively guide patients over these hurdles.
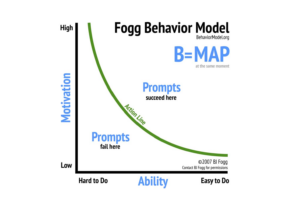
Initiating this process involves educating our patients about the benefits of healthier behaviors. The Fogg Behavior Model, developed by Dr. BJ Fogg at Stanford University, proves instrumental here. It’s a straightforward yet powerful tool that underscores the importance of both motivation and capability in instigating behavior change through innovative methods.
Imagine this scenario – a health-conscious individual, enlightened by a consultation with a care navigator about nutritious eating, might enthusiastically incorporate flaxseed into their diet. This isn’t just a random choice; it’s a strategic move to help manage blood pressure, backed by a clear understanding of its benefits. However, for someone less committed to healthful habits, this dietary adjustment might seem inconsequential or an unnecessary chore.
On the other hand, the proposition of committing to 30 minutes of daily physical activity could seem like a mountain too high to climb for some. But for others, already motivated and cognizant of its profound impact on overall health, they might welcome this change like a long-lost friend.
 This underscores the importance for care managers to effectively “read the room,” discerning which recommendations would be most acceptable to patients. They must shed light on the benefits of adhering to the care plan, while also artfully outlining the potential risks if they don’t comply. The key here is determining what each patient can easily understand and conveying this information with just the right degree of subtlety to engage them effectively.
This underscores the importance for care managers to effectively “read the room,” discerning which recommendations would be most acceptable to patients. They must shed light on the benefits of adhering to the care plan, while also artfully outlining the potential risks if they don’t comply. The key here is determining what each patient can easily understand and conveying this information with just the right degree of subtlety to engage them effectively.
In this regard, there are three applied elements of the Fogg principle to consider:
- Regular Communication as Motivation: It’s crucial to remember that patients should not only be contacted when remotely monitored measurements are trending out of range. Regular communication is key, particularly when their health metrics are improving. Encouraging words and virtual high-fives from healthcare providers can significantly boost their motivation. After all, who doesn’t appreciate a bit of commendation for reaching their health milestones? This approach underscores the importance of acknowledging every step, no matter how small, in their journey towards improved health. It’s about applauding the wins along the way, promoting a positive mindset, and strengthening their commitment to managing their health effectively.
- Ability: The ‘can do’ part of the equation. It’s important to ensure our patients feel confident in using the tools we provide for monitoring their health. This means choosing user-friendly tech, offering clear instructions, and standing by to offer help when needed. And let’s not forget – every patient is different, so our approach needs to be tailored to suit their physical and cognitive abilities.
- Occasional Prompts as Triggers: Lastly, in virtual care, it is vital to employ the occasional prompt, particularly when patients haven’t transmitted data in a few days or have missed consultations. For those where it’s feasible, this typically takes the form of a text message. Consider this a gentle nudge to help patients get back on track. It might be a friendly reminder to take their medication, a timely alert to check their blood sugar, or a notification for their next virtual consult. These nudges can take various forms, such as text messages, emails, app notifications, and other methods, with the goal of using technology effectively to keep patients engaged and proactive in their care.
By understanding and applying the Fogg Behavior Model, we can create a more engaging and effective strategy for remote patient monitoring and chronic care management. It’s all about motivating patients, making it easy for them, and giving them timely nudges along the way. This way, we can help them feel valued, supported, and ready to commit to healthier habits.
Drawing Parallels: Applying Lessons from Wellness Center Management to Enhance Patient Engagement
It shouldn’t feel like rocket science, yet convincing patients, indeed people in general, to commit to a lifestyle change often seems as complex as a moon landing. Ask any gym owner about the New Year’s resolution rush—come early January, their establishments resemble bustling beehives. But by mid-February? They might as well consider converting their facilities into restaurant bars to maintain the crowd. From my experience, there are two chief culprits: 1) pushing clients too hard, as if expecting them to reach their goals overnight, and 2) insufficient motivation to stick with the plan.
During my tenure managing a wellness center with 5,000 members and a staff of 250, we tackled these hurdles head-on. Our primary mission? Optimizing retention. And guess what? In one quarter we boosted it by over 300% (comparing personal training retention to previous years).
The key is education—it fuels motivation. Each advertisement for personal training or nutrition counseling carried a potent educational message about the benefits. We used compelling, and cited statements like: “Personal training clients accomplish more in 4 weeks than those training solo for a year.”
Another crucial aspect was making workouts comfortable and achievable. My directive to the training staff was simple: ensure every newcomer leaves the club brimming with more energy than when they arrived. Get them moving, shower them with praise, and send them off buzzing with energy. Instead of staggering back to bed, beaten and bruised, they depart with a sense of accomplishment and confidence.
By adhering to these principles, our new members were not only more motivated but also found their goals within reach. The final ingredient in this recipe for success was fostering a welcoming environment. The top priority for every employee was to befriend. Greet everyone with a warm “hello” and a smile. After all, who wouldn’t want to return to a place where they’re greeted by a friend?
Similarly at HealthSnap, we’ve always recognized that the cornerstone of our success is patient engagement. Our strategies are only as effective as the overall patients experience. Here’s how we are currently applying the above principles:
- Every interaction with a patient is positive, engaging, and friendly. We ensure patients comprehend that we’re on their team, and our objective is to function as an extension of their provider to enhance their lives.
- We rely on education as our primary catalyst for inspiration and motivation, taking care not to overwhelm them. Our remote care navigators are enthusiastic educators of the care plan, always ready to provide friendly guidance.
- We steer clear of overkill. Instead of sounding like a coach who recycles the same motivational speech before every game, we judiciously “pick our spots”. A monthly consult, occasional contacts triggered by alerts, and our readiness to answer patient queries whenever they arise, ensures sustained patient engagement.
- We suggest manageable tasks: relatively brief, interactive live sessions to discuss physician-prescribed care plans and remotely taken measurements. Additionally, we offer easy-to-follow, evidence-based lifestyle strategies to aid patients in combating disease and leading healthier lives. Just like the approach at the wellness center, our aim is to make the process comfortable, achievable, and enjoyable for the patients.
Embracing Change: Applying the Transtheoretical Model to Enhance Patient Engagement in Remote Monitoring and Chronic Care Management
A third principle to consider when aiming for a patient-centered solution is the Transtheoretical Model (TTM), better known as the stages of change model. This model acts as an invaluable guide for patients navigating their health journey, recognizing that readiness to change can fluctuate and that each individual progresses at their own pace. Therefore, it is important to understand how each stage can be incorporated into patient consultations for remote patient monitoring and chronic care management:

- Precontemplation: At this stage, patients may not realize they need to make changes to manage their chronic conditions better. The role of the care navigator is to raise awareness about their health status and the benefits of effective management. This could involve sharing educational materials or success stories from other patients.
- Contemplation: At this stage, patients are aware they need to make changes but may feel ambivalent. Here, we can encourage them by discussing the pros and cons. It’s important to highlight that even the most subtle lifestyle changes can have a significant impact, particularly for those starting with less-than-optimal habits. We can also reassure them that it’s normal to feel uncertain and that we’ll support them every step of the way.
- Preparation: Patients at this stage are ready to take action. We can help them set realistic goals and create a detailed plan. This might include deciding what tools they’ll use for remote monitoring, scheduling regular check-ins, and identifying potential barriers and ways to overcome them.
- Action: This is where patients start implementing their plan. As digital healthcare providers, we can provide ongoing support and feedback. For example, we could offer interactive live sessions each week where patients can take measurements and discuss lifestyle strategies. This approach ensures regular engagement without overwhelming them.
- Maintenance: At this stage, patients have been managing their condition effectively for a while. Our goal is to help them maintain these behaviors. We can do this by continuing to provide support, celebrating their progress, and helping them navigate any challenges that come up.
- Termination: The ultimate goal is for patients to reach this stage, where healthy behaviors have become a part of their daily routine. However, it’s important to remember that relapses can happen, and it’s our job to help patients get back on track if they do.
By incorporating the TTM into our approach, we can meet patients where they are and provide tailored support. This not only enhances patient engagement but also sets us apart from competitors. It’s about more than just providing a service; it’s about empowering patients to lead healthier lives. And with the right approach, we can make this mission a reality.
Summary
Effectively engaging patients in their healthcare journey necessitates a fusion of psychological insights and strategic implementation. By leveraging principles such as the Yerkes-Dodson inverted U theory, the Fogg Behavior Model, and the Transtheoretical Model, we can customize our approaches to cater to each patient’s unique needs and readiness for change. These models assist in finding the right balance between motivation and capability, guiding patients through their health journey at a pace that suits them best. In a manner akin to managing a successful wellness center, fostering a supportive and welcoming environment within digital healthcare strategies can significantly boost patient engagement. The ultimate goal is to empower patients, aiding them in adhering to their care plan and managing their conditions more effectively, thereby enhancing their quality of life.
HealthSnap’s Virtual Care Management Programs Take a Patient-Centered Approach
The growing role of Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) software companies represents a significant shift toward patient-centered, comprehensive care for individuals with chronic conditions.
One of the key metrics to assess the capability and performance of a virtual care management company, HealthSnap has emerged as an industry leader in Chronic Care Management (CCM) and Remote Patient Monitoring (RPM) technology and services. HealthSnap is more than just an integrated virtual care platform– we’re a proven solution to bring a higher quality of life to people with chronic conditions and their care teams.
To learn more about how our integrated Virtual Care Management Platform can help drives a patient-centered approach to care, contact us today at 888-780-1872 or click here to schedule a demo.











