By Wesley Smith, PhD and Craig Flanagan, PhD
When HealthSnap was founded to use emerging technology, such as wearable and home devices, as a proactive style of care designed to integrate with care plans and disease management, we expected to make a difference—of course—but it’s making a difference more than we had imagined. We came up with the concept before Remote Patient Monitoring (RPM) was a strategy approved by CMS for physician reimbursement. Nearly a decade later, in 2024, HealthSnap collected an average of 1.7 patient data transmissions per second. To say “the data is in” is a vast understatement. There is no doubt that RPM is transforming how we manage chronic health conditions, and it should be the new standard of care, especially for the approximately 100 million Americans suffering from cardiometabolic disease. From tracking blood pressure at home to sending real-time glucose readings to care teams, RPM helps patients get healthier—without needing constant trips to the doctor’s office—reducing adverse events, ER visits, hospitalizations, and lowering costs. The more patients transmit data as part of their daily routine, the better they do, but how much data is truly “enough” to make a significant difference?
Recent analyses show that when it comes to improving blood pressure and blood sugar, even just a few data transmissions per 30-day period can have significant and clinically meaningful benefits and are associated with major improvements in health.
Blood Pressure Improvements Without the Overload
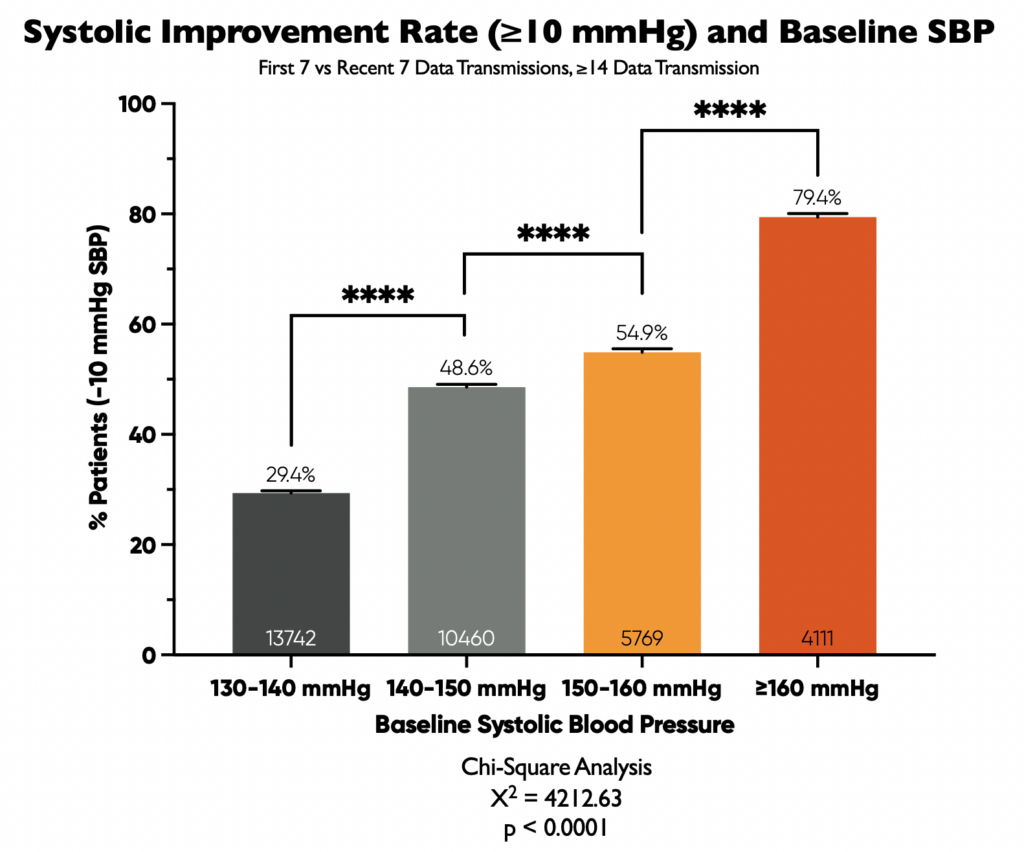
We looked at over 34,000 patients using cellular-enabled home blood pressure monitors (no need for apps or Bluetooth connectivity). Among these, 20,658 patients had a baseline systolic blood pressure (SBP) of 140 mmHg or higher, calculated as the average of their first seven blood pressure readings. This data was securely transmitted to electronic medical records, allowing for real-time monitoring by healthcare providers.
We then compared the initial SBP (the average of the first seven readings) to the most recent SBP (the average of the last seven readings) to see how the frequency of data transmission impacted blood pressure improvement.
Why 10 mmHg Matters
We focused on patients achieving a reduction of at least 10 mmHg in their SBP because a 10 mmHg reduction is a well-established benchmark associated with some serious health benefits, including:
- A 20% reduction in major cardiovascular events
- A 27% lower stroke risk and 28% lower heart failure risk
- A 17% lower coronary heart disease risk
- A 13% reduction in all-cause mortality
Basically, a 10 mmHg drop can significantly improve your health outcomes.
What the Numbers Say
Our study revealed a significant connection between initial blood pressure levels and the likelihood of achieving that crucial 10 mmHg reduction.
Key Findings:
- Higher Starting Point, Bigger Drop: Patients with higher baseline SBP values were significantly more likely to achieve a 10 mmHg or greater reduction.
- Benefits for Everyone: Even patients with lower baseline SBP (130-140 mmHg) saw improvements, with nearly 30% achieving the 10 mmHg benchmark.
A statistical analysis (Chi-Square analysis, if you’re into the science: X² = 4212.63, p < 0.0001) confirmed the strong relationship between baseline SBP and the likelihood of achieving a significant reduction.
Digging Deeper: How Often is Often Enough?
We also explored the relationship between how often patients transmitted their blood pressure data and the resulting improvements. While a detailed analysis (nonlinear regression model, R² = 0.016) showed only a weak direct correlation between transmission frequency and SBP improvement, some interesting insights emerged.
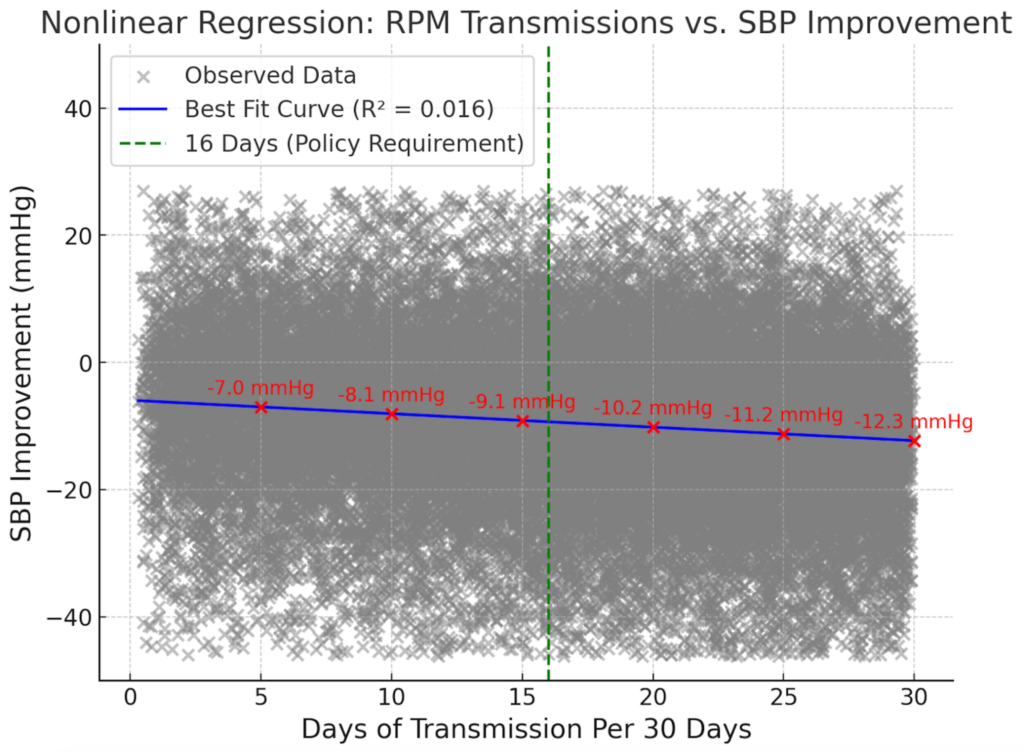
Key Observations:
- Even a Little Helps: Clinically meaningful blood pressure reductions were seen across all transmission frequencies, even when patients transmitted data as infrequently as 1-3 days per 30-day period.
- More Isn’t Always More (Directly): The weak correlation suggests that other factors play a significant role in RPM’s success. These include:
- Real-time clinical decision-making, thanks to continuous BP data access.
- More reliable blood pressure trends from home monitoring compared to in-office readings.
- Improved care plan adherence and medication compliance driven by RPM interventions.
- Increased patient self-efficacy and understanding of their health through regular clinical interactions.
- Timely clinician responses triggered by customizable alert thresholds.
So basically, it’s not just the data, it’s what you do with it.
The Sweet Spot: Finding the Right Balance
Figure 3 illustrates the strong relationship between the frequency of data transmission and improvements in SBP among 20,658 patients with uncontrolled hypertension (baseline SBP ≥140 mmHg). The results show a clear dose-response pattern: patients who transmitted data 16 or more days per 30-day period – the current threshold for RPM reimbursement under CPT code 99454 – experienced the greatest SBP reduction (–16.0 mmHg, from 151.9 mmHg to 135.9 mmHg).
However, substantial improvements were also observed in patients who transmitted fewer than 16 days per month and are currently ineligible for reimbursement. Even those transmitting data just 1–3 days per month saw a –9.3 mmHg reduction in SBP, while those in the 9–12 day and 12–15 day groups achieved reductions of –12.5 mmHg and –13.1 mmHg, respectively.
This compelling trend highlights the potential benefits of engaging more patients in RPM—even those who do not meet the current billing criteria.
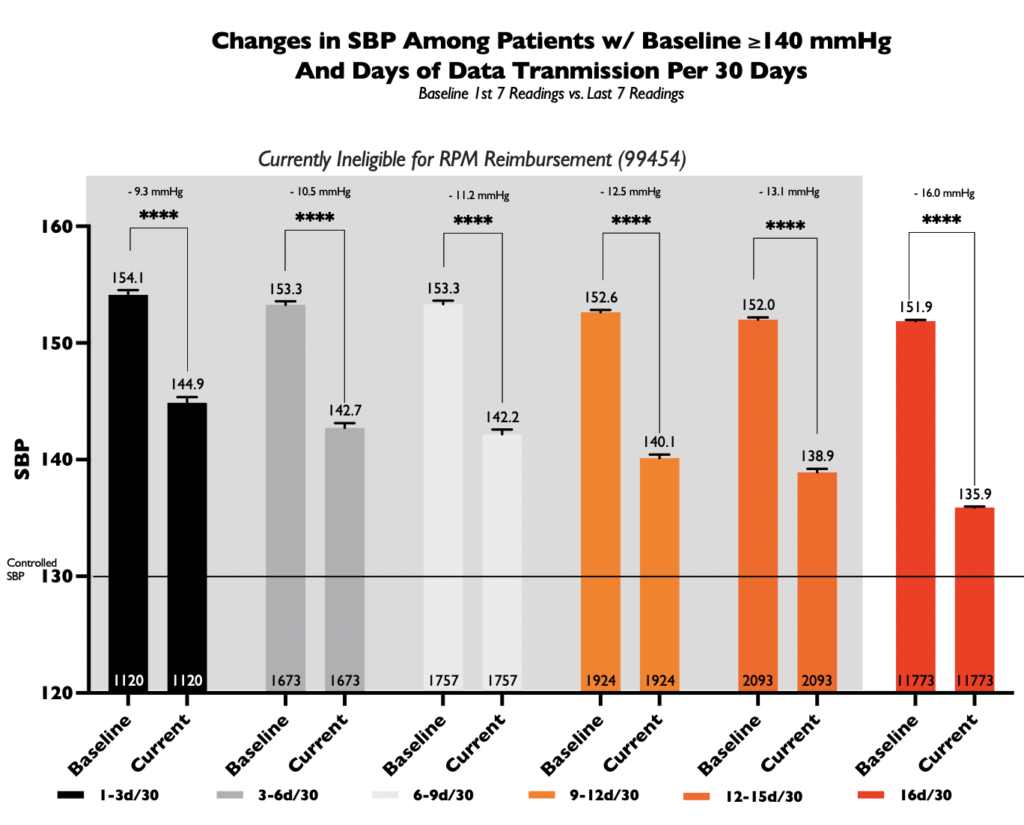
The Takeaway
This analysis reinforces the clinical value of Remote Patient Monitoring in hypertension care. A reduction of just 5–10 mmHg in SBP is associated with significantly lower risk of cardiovascular events, including stroke and heart attack. Yet the data from Figure 3 show that many patients fall just short of the 16-day threshold—while still achieving meaningful clinical improvements.
Expanding access to RPM for patients transmitting fewer than 16 days per month could unlock significant public health gains, enabling more individuals to control their blood pressure while potentially lowering long-term healthcare costs
Blood Sugar Tells the Same Story
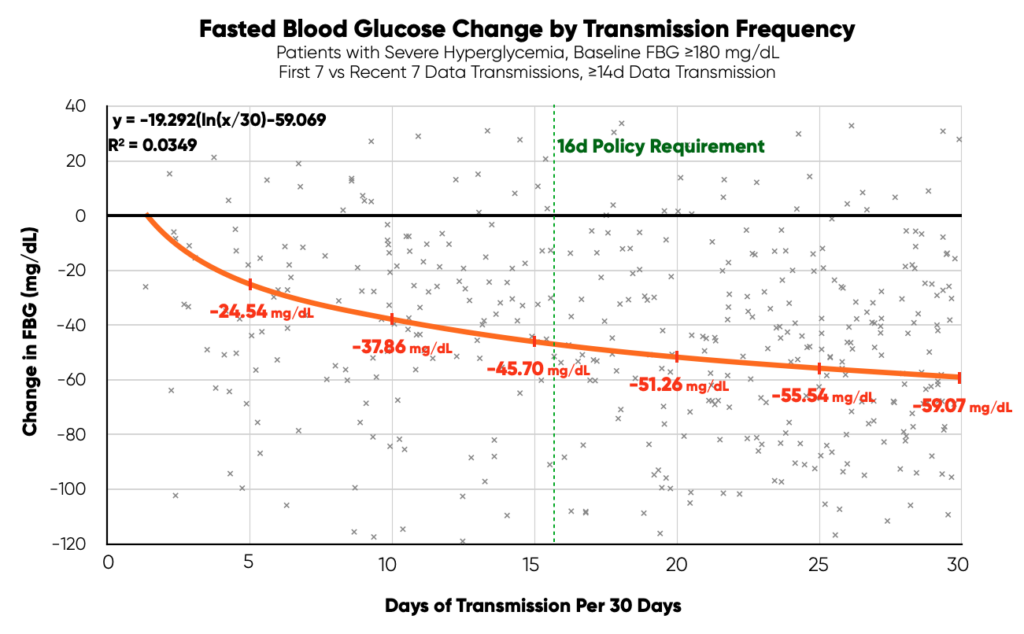
We also analyzed 501 patients with high fasting blood glucose (FBG)—diabetics with severe hyperglycemia averaging 180mg/dl across their first 7 days of data transmission. Again, even moderate RPM use made a big difference:
- 5–10 transmissions per 30-day period led to a nearly 38 mg/dL drop in FBG
- 10–15 transmissions dropped levels by nearly 46 mg/dL
And yes, more data (16+ transmissions) was best—but gains started to level off. This pattern suggests there’s a threshold effect: early and moderate engagement delivers strong results, and piling on more data doesn’t automatically lead to better health. Interestingly, these patients seeing clinically meaningful reductions between 5 and 15 days per 30-day period are not meeting the criteria for CMS reimbursement.
What This Means for the Future of RPM
The takeaway is simple: engagement matters, not just the number of data points. The current assumption that patients must submit data 16 or more days per 30-day period may overlook the bigger picture.
RPM’s power lies in:
- Making care more proactive
- Helping patients understand their bodies
- Encouraging small, consistent habits and medication compliance
- Letting clinicians intervene early
Whether it’s managing hypertension or improving glucose control, even modest RPM participation can be a game-changer.
Bottom Line
Technology doesn’t need to be overwhelming to be effective. These findings remind us that the value of RPM isn’t just in the numbers—but in the connection it fosters between patients and their care teams.
As we look to the future, the goal should be to maximize patient outcomes, not just check off boxes. That means making RPM more flexible, more accessible, and focused on what truly drives health: partnership, engagement, and personalized care.
To learn more about the HealthSnap RPM solution, please book time with our team here.