By Wesley Smith, Ph.D., HealthSnap Co-Founder & Chief Scientific Officer
Where RPM Shines
Remote Patient Monitoring (RPM) is primarily designed to manage chronic conditions, going beyond serving as a simple life-alert system for emergencies. The true potential lies in transforming healthcare for the nearly half of Americans dealing with hypertension and the staggering number of individuals, nearly 100 million, facing glucose stress. Moreover, the remote nature of this technology helps address the disparities in healthcare accessibility across the country. The impact of RPM extends far beyond emergency alerts and has the potential to bring about a revolution in healthcare delivery.
Now this is not to say that Remote Patient Monitoring is unable to play a vital role in responding to critical values and potentially life-saving interventions, especially when combined with tools like pulse oximetry or used for monitoring rapid weight changes in conditions such as Heart Failure (HF) or Chronic Kidney Disease (CKD). However, it is crucial not to oversimplify its utility, as doing so may inadvertently create misconceptions about the true power of the intervention, which we at HealthSnap believe is the future of healthcare.
Addressing Potential Misconceptions
Viewing Remote Patient Monitoring as an “emergency response system” can be risky if not properly explained to patients. Consider an elderly patient using RPM who might think they’re being constantly “monitored”. If they experience symptoms such as chest pain or a Transient Ischemic Attack (TIA), and don’t receive an immediate callback after measuring their vitals, they might incorrectly assume that everything is okay and neglect to seek necessary medical attention.
This scenario underscores the need for clear communication about the purpose and limitations of Remote Patient Monitoring to each patient. It also supports the argument for using RPM mainly for chronic condition management rather than solely as an emergency alert system. By adopting this approach, we can use Remote Patient Monitoring to encourage preventative care and proactive health management.

The Power of Disease Management and Event Prevention
Having access to one’s health data can be a transformative form of augmented feedback, enhancing both meta-cognition and self-efficacy. This process allows individuals to gain a deep understanding of their health status, identify patterns, and make informed decisions about their behaviors. Essentially, by providing a clear snapshot of their current health state (rationale for the name HealthSnap), this feedback empowers individuals to take control of their well-being, strengthening their belief in their ability to bring about positive clinical change. This aspect of self-efficacy is vital for improving outcomes across the myriad of recognized chronic conditions.
The Proven Impact of Home Monitoring and Blood Pressure Reduction
When it comes to RPM, the most prevalent use-case is its application in managing hypertension. We can gain valuable insights into its effects by examining various scientific studies. For instance, a meta-analysis published in The Lancet in 2021 by Rahimi et al., involving nearly 350,000 patients, revealed that even a modest reduction of 5 mmHg in Systolic Blood Pressure (SBP) can lead to a significant 10% decrease in serious cardiovascular events.
Additionally, a study by Tucker et al., published in PLoS Medicine in 2017, demonstrated that regular home-based monitoring could lower systolic pressure by 3 mmHg, highlighting the potential of Remote Patient Monitoring in managing hypertension and mitigating the risk of cardiovascular events. However, when implemented correctly, RPM has the power to surpass these numbers altogether.

Harnessing the True Potential of Remote Patient Monitoring
In the realm of digital healthcare, HealthSnap is making remarkable strides with its pioneering outcomes. Within just 90 days of implementing HealthSnap’s digital care treatment, hypertension patients witnessed an average drop in systolic blood pressure of 10 mmHg. Even more astonishingly, patients diagnosed with Stage 2 Hypertension experienced an average reduction of 18.3 mmHg (p < 0.0001).
What truly sets these outcomes apart is their sustainability. After one year of treatment, the average systolic improvement remained consistent at 13.6 mmHg for all hypertensive patients. For those grappling with Stage 2 hypertension, the average systolic improvement skyrocketed to 21 mmHg (p < 0.0001), underscoring the long-term efficacy of a properly delivered Remote Patient Monitoring approach.
These results caught the attention of the wider medical community and were proudly presented at the Hypertension 2023 Scientific Sessions Conference hosted by the American Heart Association. Among Stage 2 patients from cardiology clinics, systolic pressure improved by 21 mmHg and diastolic pressure by 14 mmHg. Primary care patients diagnosed with Stage 2 hypertension also experienced significant improvements, with systolic and diastolic pressures showing respective changes of 16 mmHg and 10 mmHg (p < 0.0001).
These extraordinary outcomes highlight the transformative potential of properly administered Remote Patient Monitoring treatment in effectively managing hypertension and enhancing patient health outcomes over time.
Consider, for instance, the remarkable improvements witnessed among Stage 2 hypertension patients utilizing HealthSnap’s programs across various client groups.
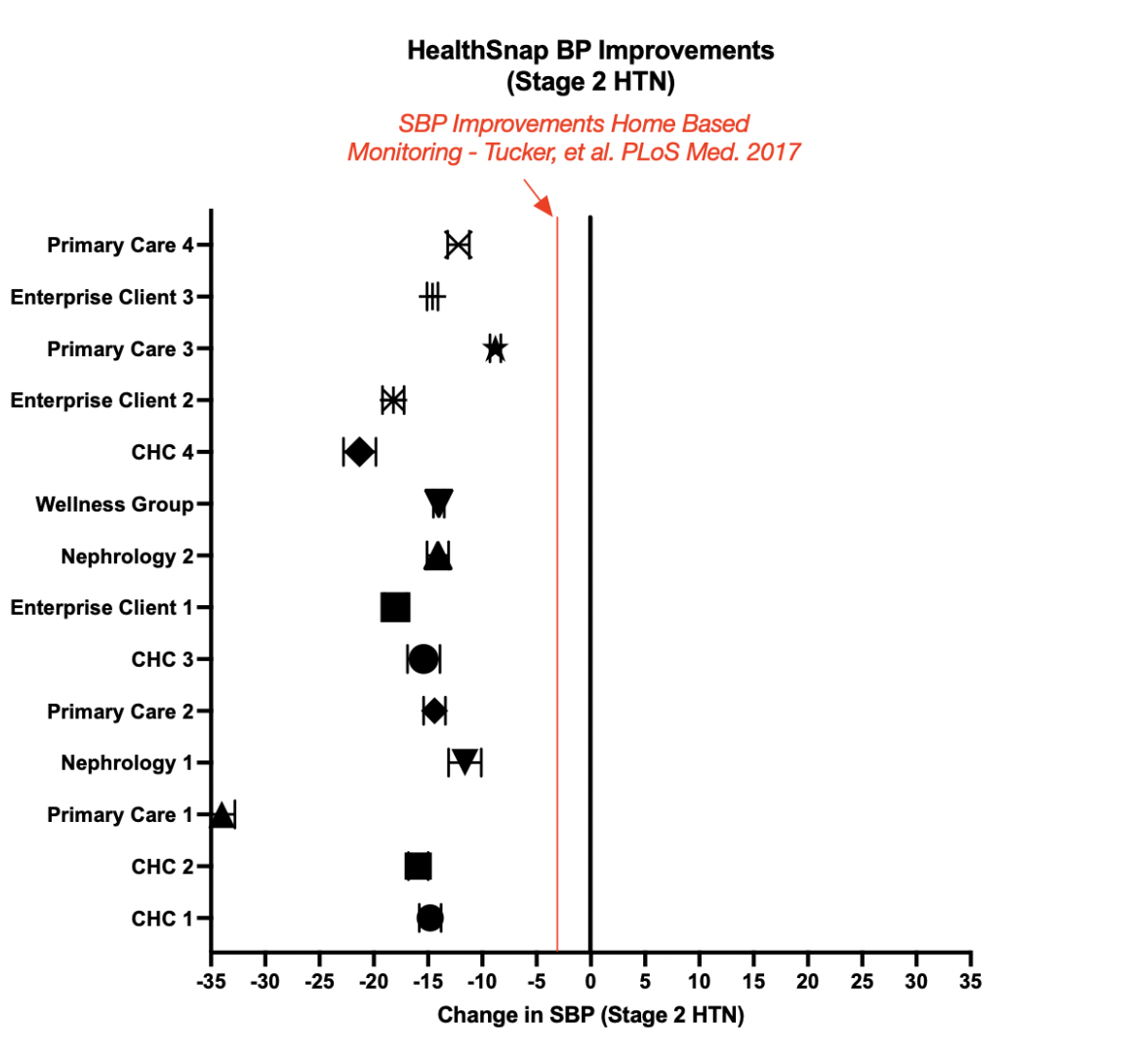
FIGURE 1: Improvements among categories of HealthSnap clients in Stage 2 Hypertension patients (p < 0.0001; N over 20,000 patients)
Mastering the D.O.M.A.I.N of Remote Monitoring & Disease Management
One of the most important emerging roles in healthcare is that of the care navigator. These remote clinical staff members are trained to provide a concierge-style of remote care, ensuring equitable healthcare for all patients, regardless of their socioeconomic status. They play a crucial role in establishing effective communication and continuity of care, addressing the gaps often experienced in traditional medicine. The training and operation of these care navigators on the front lines of patient monitoring are essential to the success of the program. At HealthSnap, our care navigators are trained to master their D.O.M.A.I.N when dealing with Remote Patient Monitoring patients, and this acronym serves as the centerpiece of their patient consultations.
The “D” stands for data. Data is the foundation of Remote Patient Monitoring, as it provides valuable insights into the patient’s physiological variables over time. During consultations, it is crucial to focus heavily on data trends, helping patients gain the most benefit from understanding their own physiology. By using the data, patients can make informed decisions about their lifestyle strategies and improve their health literacy. This is similar to how a marathon runner uses heart rate monitor targets to achieve desired performance outcomes. For example, patients may discover that skipping medication on certain days has a negative impact on their measurements. They may realize that lack of sleep significantly affects their blood pressure, or that stressful days have a profound effect on their glucose levels. On the other hand, they might find that being more physically active improves their measurements. The possibilities are endless, and a significant part of the consultation should be dedicated to helping patients recognize and understand these changes.

The “O” is an equally significant component of the acronym, representing “obtaining reliable measures.” Consider the scenario where a patient measures their blood pressure at different times of the day, under varying conditions – sometimes in the morning after a 5-minute relaxation period, other times while rushing out the door to work, occasionally medicated, and occasionally not. In such cases, the measurements will be inconsistent and unreliable, making it nearly impossible to use the data effectively for clinical decisions, adjustments, or meaningful analysis of clinical improvements or predictive analytics. To ensure the data can be properly used, it is essential to standardize the process of obtaining measurements in a consistent and reliable manner, much like incorporating it into the patient’s daily routine. For example: Wash your face. Brush your teeth. Take your medication. Sit down and relax. Take your blood pressure. At HealthSnap, our care navigator nurses place great emphasis on this aspect, enabling us to use Remote Patient Monitoring data to support informed clinical adjustments by providers and for the development of fascinating predictive analytics and insights.
The “M” in the acronym squarely focuses on medication compliance and reconciliation. It involves accurately charting and communicating information about the medications related to the variable being measured. This step is critical because patients may experience improvements that require adjustments to their medications. Furthermore, when it comes to Remote Patient Monitoring care coordination, the focus should solely be on the medications related to the variable being discussed. Interestingly, we find that the RPM discussion and the power of educating patients through their physiological data are among the best ways to improve treatment adherence and medication compliance.
The “A” represents the opportunity for the care navigator to ask patients to “Assess” the effectiveness of the program. Patients become more effectively engaged in technology and remote care when they aren’t over-coached or intimidated. The “Approach” must be patient-centered, and as we often say at HealthSnap, care navigators should act as a “Guide on the Side,” not a “Sage on a Stage.” The program is designed for the patient’s health, and they are the ones we serve, not the other way around. Unfortunately, patients often feel this is missing in traditional healthcare settings.

The “I” in DOMAIN stands for “integrative lifestyle strategies.” HealthSnap is dedicated to using evidence-based lifestyle recommendations for patients. However, it’s crucial for Care Navigator Nurses to understand the patient well enough to know what is palatable to them. For example, the word “exercise” may be intimidating, so it might be better to discuss the effects of regular activity or movement. It’s possible that some patients have no intention of changing anything about their diet or lack the ability to make significant changes in their eating habits. This is where proper training on the transtheoretical model of behavior change becomes critical. By recognizing the patient’s willingness to change, care navigators can consult with the right tone. Sometimes, subtle changes can make a world of difference. In fact, the worse a patient’s lifestyle is at baseline, the more dramatic the improvement small adjustments can make. This is particularly exciting when working with extremely sedentary patients with poor diets. Effective communication and motivation, presented subtly and tactfully, can bring about significant positive changes.
Lastly, the “N” in the training acronym stands for scheduling and reminding the patient of their “next appointment.” As mentioned earlier, Remote Patient Monitoring is designed to manage chronic conditions and is most effective when it becomes a regular part of the patient’s lifestyle. It’s important that they recognize it as a beneficial service and look forward to the next conversation with their care navigator, rather than seeing it as a burden. Overall, when delivered properly, RPM can reduce the need for in-person appointments and overall healthcare utilization. This is something patients may come to view as a privilege, especially if they form a meaningful bond with their care navigator.
Unleashing the Power of Remote Patient Monitoring with the DOMAIN Approach
In summary, when implementing RPM, it is crucial to master your DOMAIN. The DOMAIN approach consists of data discussion, obtaining reliable measures, medication discussion, assessment of effectiveness, integration of lifestyle strategies, and next appointment.
By focusing on these key components, healthcare providers can ensure a successful Remote Patient Monitoring program implementation. Accurate data collection, ongoing communication and support, use of technology, patient assessment and engagement, integrative lifestyle strategies, and effective appointment scheduling are all essential aspects to excel in the realm of remote care. Mastering their DOMAIN empowers healthcare professionals to confidently navigate the complexities of RPM and provide optimal care for patients with chronic conditions, exceeding expectations compared to routine home measurements.






