Virtual Care Management Programs, specifically Remote Patient Monitoring (RPM) and Chronic Care Management (CCM), have emerged as powerful tools to enhance clinical workflows and improve patient outcomes. Healthcare providers and hospitals are increasingly recognizing the transformative potential of these programs, leveraging technology to bridge the gap between in-person visits and continuous, proactive care. In this guide, we will discuss the profound ways in which RPM and CCM can improve clinical workflows, offering healthcare professionals a more innovative and effective approach to patient care.
Role of Virtual Care Management Programs in Healthcare
Continuous Patient Monitoring with RPM
Remote Patient Monitoring, a cornerstone of modern healthcare, enables healthcare providers to monitor patients’ vital signs and health metrics in near real-time. By integrating RPM into clinical workflows, healthcare professionals can access a continuous stream of patient data, fostering early detection of deteriorating health conditions and preventing hospital readmissions. The seamless transmission of vital information allows for timely interventions, reducing the burden on emergency departments and encouraging a proactive approach to patient care.
Enhanced Care Coordination through CCM
Chronic Care Management programs focus on providing comprehensive, continuous care for patients who have 2 or more chronic conditions, fostering a collaborative approach among healthcare providers. By incorporating CCM into clinical workflows, healthcare teams can establish personalized care plans, coordinate services, and engage in proactive communication with patients. This not only improves patient adherence to treatment plans but also enhances the overall quality of care, leading to better health outcomes.
Efficiency and Time Management
Virtual Care Management Programs streamline clinical workflows, optimizing time management for healthcare providers. By automating routine tasks such as appointment reminders, medication adherence checks, and health status assessments, RPM and CCM allow clinicians to allocate their time more efficiently, focusing on complex patient cases and critical decision-making.

Data-Driven Decision Making
The wealth of patient data generated through RPM and CCM facilitates data-driven decision-making. Healthcare providers can analyze trends, identify risk factors, and tailor interventions based on individual patient needs. This data-driven approach enhances the precision of diagnoses and treatment plans, fostering a more personalized and effective healthcare delivery system.
Patient Engagement and Empowerment
Virtual Care Management programs actively involve patients in their care journey. Through secure patient portals and mobile applications, individuals can access their health data, receive educational resources, and communicate with their healthcare team. This increased engagement fosters a sense of empowerment, encouraging patients to take an active role in managing their health and making informed decisions.
Remote Accessibility
Remote Patient Monitoring (RPM) and Chronic Care Mangement (CCM) break down geographical barriers, enabling healthcare industry providers to deliver care remotely. This is especially crucial in reaching underserved populations and patients in rural areas. Virtual care programs facilitate regular check-ins, reducing the need for frequent in-person visits and ensuring that patients receive consistent, high-quality care irrespective of their location.

Billing and Reimbursement Opportunities
The integration of RPM and CCM into clinical workflows presents healthcare providers and hospitals with new billing and reimbursement opportunities. As these programs match with value-based care models, providers can leverage the additional services offered through RPM and CCM to enhance revenue streams while delivering enhanced patient care.
What are Clinical Workflows?
Clinical workflows refer to the series of tasks, processes, and procedures that healthcare professionals follow to deliver patient care within a healthcare setting. These workflows encompass the entire patient journey, from initial contact and assessment to diagnosis, treatment, and follow-up.
Clinical workflows are designed to optimize the efficiency and effectiveness of healthcare delivery, ensuring that each patient receives comprehensive and coordinated care. They involve the collaboration of various healthcare providers, including physicians, nurses, technicians, and administrative staff, each contributing to different stages of patient care.
Clinical workflows are critical for maintaining high-quality care, minimizing errors, and enhancing communication among healthcare team members. With the advent of technology, the integration of electronic health records (EHRs), telemedicine, and virtual care management programs has further transformed and streamlined clinical workflows, improving patient outcomes and the overall healthcare experience.
Advantages of Efficient Clinical Workflows
Efficient clinical workflows play a pivotal role in ensuring the delivery of high-quality healthcare and contribute significantly to positive patient outcomes. The importance of efficient clinical workflows can be understood through several key aspects:
Patient Care Coordination
Efficient workflows facilitate seamless coordination among healthcare providers, ensuring that patients receive timely and coordinated care. From initial assessment to diagnosis and treatment, streamlined workflows enable a smooth transition between different stages of care.
Reduced Errors and Improved Patient Safety
Well-designed workflows help minimize the risk of errors in diagnosis, medication administration, and other critical aspects of patient care. By providing standardized processes and clear communication channels, healthcare professionals can work together cohesively, reducing the likelihood of adverse events.
Enhanced Communication
Efficient workflows promote effective communication among healthcare team members. This is crucial for sharing patient information, test results, and treatment plans, leading to better-informed decision-making and improved overall patient care.

Time and Resource Optimization
Optimized workflows contribute to time and resource efficiency. Healthcare providers can allocate their time more effectively, focusing on patient care rather than navigating complex and cumbersome processes. This efficiency also allows for better utilization of healthcare resources.
Improved Patient Experience
Patients benefit from streamlined workflows through reduced waiting times, faster access to care, and a more organized healthcare experience. This contributes to higher patient satisfaction and engagement in their own healthcare journey.
Adaptability to Technological Advances
As healthcare continues to integrate technology, efficient workflows facilitate the seamless incorporation of electronic health records (EHRs), telemedicine, and virtual care management programs. This adaptability ensures that healthcare providers can leverage technological advancements to improve patient care.
Regulatory Compliance
Many healthcare regulations and standards emphasize the importance of well-defined and documented clinical workflows. Efficient workflows help healthcare organizations adhere to these regulations, ensuring compliance with standards such as HIPAA and promoting a culture of accountability.
Data Management and Analysis
Streamlined workflows contribute to effective data management, allowing healthcare providers to collect, store, and analyze patient data more efficiently. This data-driven approach supports evidence-based decision-making, leading to better patient outcomes.
Challenges that May Disrupt Traditional Clinical Workflows
Clinical workflows are essential for the effective functioning of healthcare systems, but they often face various challenges that can impact efficiency and patient care. Some common challenges in clinical workflows include:
Increasing Complexity of Care
The evolving landscape of healthcare introduces new treatment modalities, advanced technologies, and a growing understanding of complex medical conditions. Managing the increasing complexity of care requires healthcare professionals to stay updated on the latest advancements, which can be time-consuming. Integrating these complexities into clinical workflows without causing disruptions is a challenge that healthcare systems face in providing optimal patient care.
Healthcare Staffing Shortages
Shortages in healthcare staffing, including physicians, nurses, and support staff, pose a significant challenge to clinical workflows. Increased patient demand, especially during critical times, can overwhelm existing staff, leading to longer wait times, decreased patient satisfaction, and potential errors. Staffing shortages may also affect the implementation of new technologies or workflows, emphasizing the need for strategic workforce planning and resource allocation.
Fragmented Systems and Information Silos
Healthcare providers often use different systems for various tasks, leading to fragmented information. Lack of integration between systems can result in information silos, hindering smooth communication and coordination among healthcare professionals.
Manual and Paper-Based Processes
Many healthcare institutions still rely on manual, paper-based processes, which are time-consuming and prone to errors. Transitioning to electronic health records (EHRs) can be challenging, and resistance to change can impede the adoption of more efficient digital workflows.
Communication Gaps
Ineffective communication between healthcare team members can lead to delays in care, misunderstandings, and compromised patient safety. Communication gaps may occur during care transitions, handovers, or when using disparate communication tools.
Technological Barriers
While technology offers significant benefits, its implementation can pose challenges. Issues such as inadequate training, system downtimes, or difficulties in using new software can disrupt workflows and create resistance among healthcare professionals.

Regulatory Demands
Meeting regulatory requirements, such as those outlined by HIPAA, can be challenging. Compliance issues may arise due to a lack of standardized processes, incomplete documentation, or difficulties in keeping up with evolving healthcare regulations.
Workflow Redundancies
Inefficient workflows often involve redundant or duplicated tasks, leading to wasted time and resources. Identifying and eliminating these redundancies is crucial for optimizing workflows and improving overall efficiency.
Limited Interoperability
Incompatibility between different health IT systems can hinder interoperability. The inability to seamlessly share patient information between systems can slow down clinical workflows and compromise the continuity of care.
Resistance to Change
Healthcare professionals may resist changes in workflows, especially when transitioning to new technologies or procedures. Overcoming resistance requires effective change management strategies and continuous education and training.
Workload Pressures
High patient volumes and demanding workloads can strain clinical workflows, leading to burnout among healthcare providers. Adequate staffing levels and workload management strategies are crucial for maintaining a balance between efficiency and staff well-being.
Security Concerns
Protecting patient data is a top priority, and concerns about data security can impact the adoption of digital workflows. Ensuring robust cybersecurity measures and addressing privacy concerns are essential for building trust in digital healthcare systems.
How Remote Patient Monitoring Helps Improve Clinical Workflows
Remote Patient Monitoring (RPM) plays a pivotal role in enhancing clinical workflows by introducing innovative solutions that bridge the gap between healthcare providers and patients. Here are several ways in which RPM contributes to improving clinical workflows:
Continuous Patient Monitoring
RPM enables near real-time tracking of patient vitals and health metrics, providing healthcare providers with a comprehensive view of the patient’s health status. This continuous monitoring reduces the need for frequent in-person visits, allowing providers to focus on more critical cases and optimizing their time.
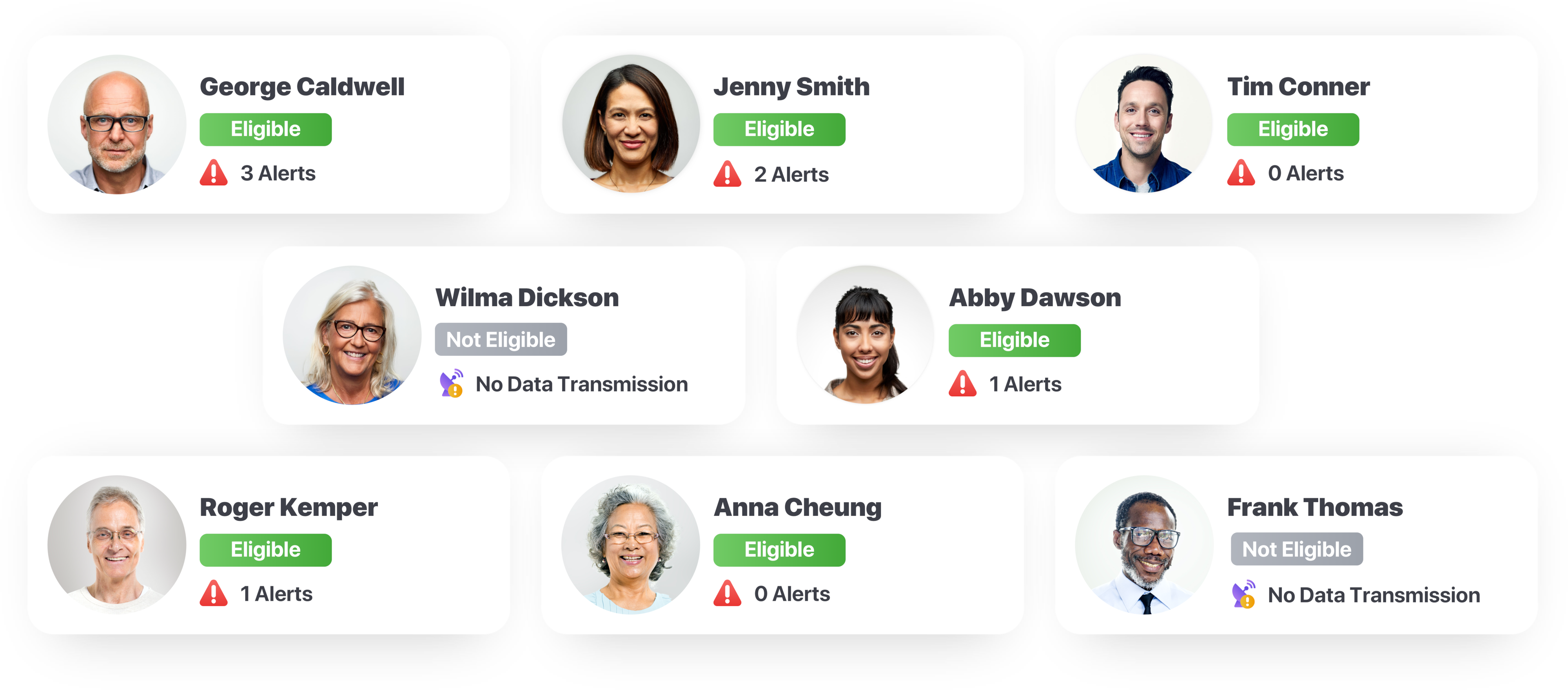
Early Detection of Health Issues
With Remote Patient Monitoring (RPM), healthcare providers receive timely alerts for any abnormal variations in patient data. This early detection of health issues enables proactive intervention, preventing the escalation of problems and reducing the likelihood of emergency hospital admissions.
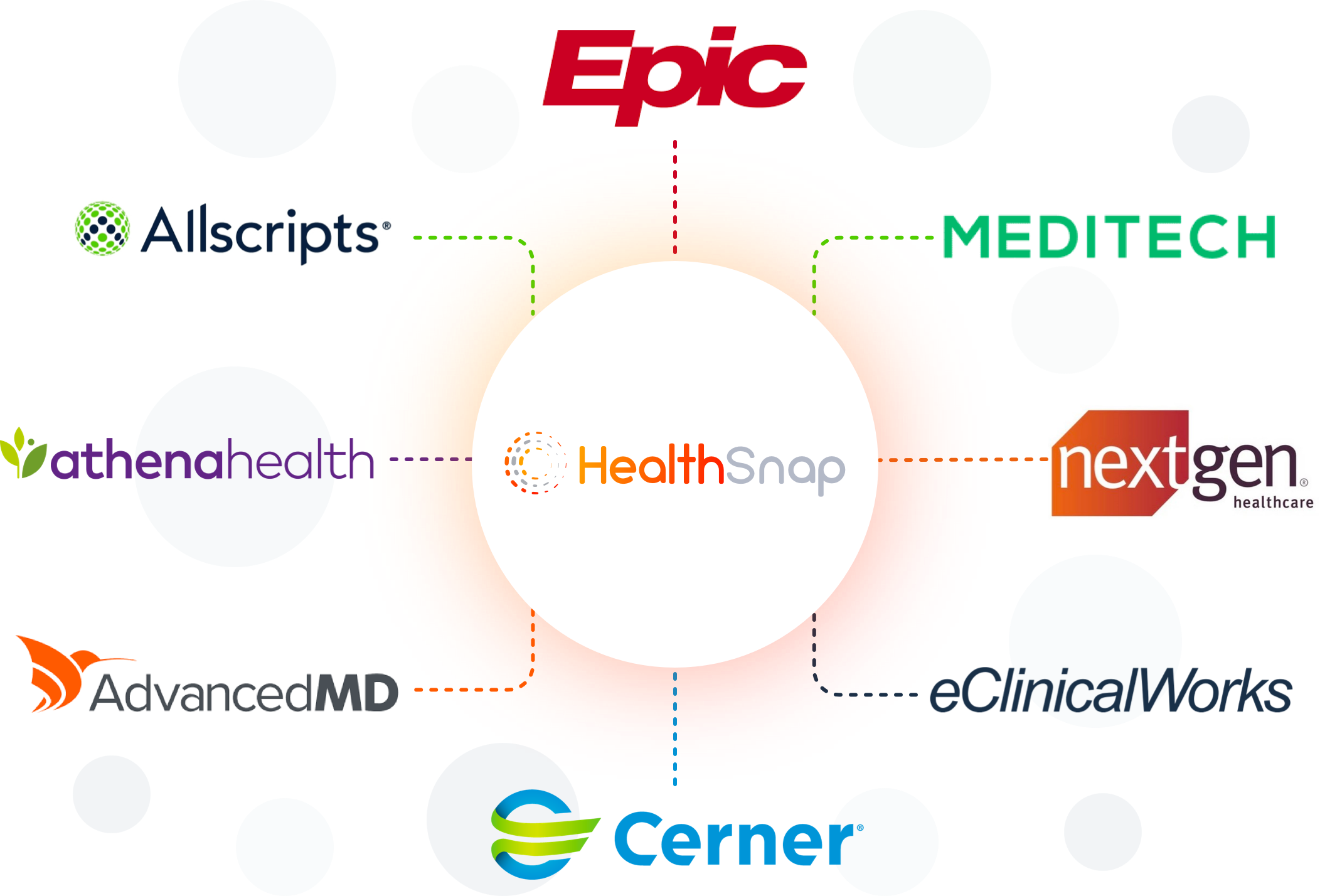
Data Integration into EHR Systems
Remote Patient Monitoring platforms seamlessly integrate with Electronic Health Record (EHR) systems, streamlining the flow of patient data into the provider’s existing workflows. This integration ensures that healthcare professionals have access to a patient’s complete medical history, facilitating more informed decision-making.
Personalized Care Plans
RPM facilitates the creation of personalized care plans based on individual patient data. This tailored approach ensures that interventions are aligned with specific patient needs, enhancing the efficacy of treatments and interventions.
Enhanced Patient Engagement
By empowering patients to monitor their health, Remote Patient Monitoring programs encourage active participation in their own care. This engagement not only improves patient outcomes but also reduces the burden on healthcare providers by fostering a more collaborative approach to healthcare management.
Optimized Resource Allocation
Through remote monitoring, healthcare providers can allocate resources more efficiently. Instead of spending time on routine check-ups, providers can focus on patients with acute needs, optimizing the allocation of human and technological resources.
Improved Follow-Up Procedures
RPM enables healthcare providers to conduct virtual follow-up appointments, reducing the need for patients to physically visit healthcare facilities. This not only enhances patient convenience but also streamlines the scheduling process for providers.

Cost Savings
The reduction in unnecessary hospital visits, timely interventions, and optimized resource allocation contribute to cost savings for both healthcare providers and patients. Remote Patient Monitoring helps in preventing complications, reducing hospital readmissions, and promoting overall healthcare efficiency.
How Chronic Care Management (CCM) Helps Improve Clinical Workflows
Chronic Care Management (CCM) is a comprehensive healthcare approach that focuses on enhancing the management of chronic conditions, offering continuous support to patients with multiple chronic health conditions. Here’s how CCM contributes to improving clinical workflows:
Holistic Patient-Centric Care
CCM emphasizes a patient-centric model, considering the patient’s overall well-being rather than addressing individual symptoms. This approach aligns with value-based care, promoting a comprehensive understanding of the patient’s health status.
Regular Monitoring and Follow-Up
Chronic Care Management involves regular check-ins and monitoring of patients with chronic conditions. Healthcare providers can track key health metrics, medication adherence, and lifestyle factors. This continuous monitoring allows for early detection of issues and timely intervention, reducing the likelihood of complications.

Care Coordination and Team Collaboration
CCM encourages collaboration among healthcare professionals, fostering a clinical research-based and team-based approach to patient care. This collaborative model involves physicians, nurses, specialists, and other care team members working together to address the various aspects of a patient’s health.
Electronic Health Record (EHR) Integration
CCM platforms seamlessly integrate with EHR systems, streamlining the documentation of patient data. This integration ensures that healthcare providers have access to comprehensive and up-to-date patient information, facilitating more informed decision-making.
Patient Education and Empowerment
Chronic Care Management programs often include educational components that empower patients to actively manage their chronic conditions. By providing resources, guidance, and support, CCM enhances patient understanding of their health, leading to improved self-management and adherence to care plans.
Risk Stratification and Targeted Interventions
CCM utilizes risk stratification to identify patients at higher risk for complications. With this information, healthcare providers can implement targeted interventions and allocate resources more efficiently, ensuring that high-risk patients receive the necessary support and interventions.
Telehealth and Remote Monitoring
CCM embraces telehealth solutions, enabling virtual visits and remote monitoring of patients. This not only enhances patient convenience but also optimizes the use of healthcare resources. Virtual consultations and remote monitoring reduce the need for in-person visits, particularly beneficial for patients with mobility or transportation challenges.
Improved Medication Management
Medication adherence is crucial for managing chronic conditions. CCM includes strategies to improve medication management, such as medication reconciliation, patient education, and regular reviews of the patient’s medication regimen. This focus on medication adherence contributes to better health outcomes.
Enhanced Preventive Care
CCM emphasizes preventive care measures, including vaccinations, screenings, and lifestyle modifications. By proactively addressing preventive care, healthcare providers can reduce the risk of complications associated with chronic conditions, leading to improved overall patient health.

Billing and Reimbursement Support
CCM programs often provide support for billing and reimbursement for the additional services offered. This financial assistance helps healthcare providers incorporate CCM into their practices seamlessly, ensuring sustained implementation.
How Remote Patient Monitoring Enhances Nurses’ Workflows
Nurses play a vital role in healthcare, and the integration of Remote Patient Monitoring (RPM) technology has significantly enhanced their workflows. Here’s a detailed exploration of how RPM positively impacts nurse workflows:
Near Real-Time Patient Data Accessibility
-
Streamlining Patient Monitoring: RPM provides care navigator nurses with near real-time access to patient data, allowing for continuous monitoring without the need for frequent in-person visits. This facilitates early detection of any concerning trends or changes in a patient’s health status.
-
Efficient Triage and Prioritization: Nurses can efficiently triage patients based on the severity of their condition by analyzing near real-time data. This prioritization ensures that critical cases receive immediate attention, optimizing the allocation of nursing resources.

Proactive Patient Management
-
Early Intervention Opportunities: Remote Patient Monitoring enables care teams to identify potential issues before they escalate, allowing for early intervention. This proactive approach helps prevent complications and reduces the likelihood of hospital readmissions.
-
Customized Care Plans: Nurses can create personalized care plans based on the continuous data collected through RPM. These plans are tailored to each patient’s unique needs, fostering a more patient-centric approach to healthcare.
Improved Patient Engagement
-
Empowering Patients: Remote Patient Monitoring encourages patients to actively participate in their care. A nurse educator can guide patients on using monitoring devices and interpreting their data, promoting a sense of empowerment and accountability for their health.
-
Enhanced Communication: RPM facilitates regular communication between case management nurses and patients. Nurses can provide timely feedback, address concerns, and offer guidance, leading to improved patient-nurse relationships and overall engagement.
Time Efficiency and Workload Distribution
-
Reduced Routine Check-Ups: With RPM, nurses can minimize routine in-person check-ups, focusing on patients who require more immediate attention. This optimizes time and allows nurses to allocate their efforts where they are most needed.
-
Efficient Workload Distribution: RPM helps distribute nursing workload more efficiently. By choosing the best remote nursing jobs and remotely monitoring multiple patients simultaneously, nurses can manage larger caseloads without compromising the quality of care.
Integration with Electronic Health Records
-
Seamless Data Integration: RPM seamlessly integrates with EHR systems, ensuring that all patient data is consolidated in one accessible location. This integration streamlines documentation processes, reducing the administrative burden on nurses.
-
Enhanced Data Accuracy: Integration with EHRs minimizes manual data entry, reducing the risk of errors. Nurses can trust that the information they access is accurate and up-to-date, supporting informed decision-making.
Tips for Implementing Virtual Care Management Programs: RPM and CCM
The successful implementation of Virtual Care Management programs in healthcare services is pivotal for delivering patient-centric, efficient, and quality care. By following these tips, healthcare providers and a healthcare system can navigate the complexities of integrating Remote Patient Monitoring and Chronic Care Management seamlessly, ultimately realizing the potential for improved patient outcomes and enhanced clinical workflows.

Conduct a Thorough Needs Assessment
Identify Target Patient Population
-
Importance of Defining Demographics: Initiating a successful Virtual Care Management program begins with a precise identification of the target patient demographic. Discuss the relevance of understanding patient characteristics, health conditions, and unique needs. Emphasize the impact of a tailored approach on program effectiveness.
-
Aligning Objectives with Patient Needs: Explore strategies for aligning program objectives with the identified patient needs. Illustrate the significance of developing interventions and care plans that directly address the challenges and requirements of the target population.
Assess Technological Readiness
-
Significance of Technological Evaluation: Highlight the critical nature of evaluating the existing technological infrastructure within healthcare settings. Discuss the importance of a comprehensive assessment to ensure the seamless integration of Virtual Care Management programs.
-
Integration with Electronic Health Records (EHRs): Explore the integration of Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) platforms with EHRs. Discuss how this integration enhances data accessibility, reduces redundancy, and facilitates a more holistic view of patient health.
Establish Clear Program Goals and Objectives
Define Measurable Outcomes
-
Necessity of Measurable Goals: Discuss the fundamental necessity of setting measurable goals and objectives for the Virtual Care Management (VCM) program. Emphasize the importance of clearly defining what success looks like and how it will be measured.
-
Examples of Outcomes: Explore tangible examples of measurable outcomes, such as improved patient adherence to treatment plans, reduced hospitalizations, and enhanced overall patient satisfaction. Illustrate how these outcomes contribute to the success of the Virtual Care Management program.
Align with Quality Metrics
-
Alignment with Established Metrics: Explore how VCM programs align with established quality metrics in healthcare. Discuss the relevance of adherence to regulatory standards and quality benchmarks in ensuring the success and sustainability of the program.
-
Impact on Reimbursement and Healthcare Quality: Discuss the broader impact of aligning with quality metrics on reimbursement structures and the overall quality of healthcare delivery. Highlight how meeting or exceeding these metrics can lead to improved financial outcomes and elevated patient care.
Ensure Regulatory Compliance
Understand Billing and Coding Requirements
-
Overview of Requirements: Provide a comprehensive overview of the billing and coding requirements specific to Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) programs. Explain the nuances and distinctions in coding for different services within these programs.
-
Importance of Compliance: Discuss the critical importance of compliance with healthcare regulations related to billing and coding. Highlight the potential consequences of non-compliance and stress the need for accurate and transparent documentation.
Train Staff on Compliance Protocols
-
Significance of Staff Training: Emphasize the crucial role of staff training in ensuring compliance with regulatory requirements. Discuss how well-trained staff can contribute to accurate coding, documentation, and overall program adherence.
-
Ongoing Education and Updates: Provide guidance on establishing a continuous education program for staff, keeping them informed about evolving regulatory changes. Share resources for staying updated on compliance protocols to foster a culture of ongoing learning within the healthcare organization.
Invest in User-Friendly Technology
Select Intuitive Platforms
-
Importance of User-Friendly Platforms: Emphasize the significance of choosing virtual care platforms that are intuitive and user-friendly. Discuss how user-friendly interfaces enhance the overall experience for both healthcare providers and patients, contributing to increased engagement and adherence.
-
Enhancing Experiences: Explore features with a proven healthcare technology company that can enhance the user experience on RPM and CCM platforms. This may include streamlined navigation, real-time data visualization, and interactive tools that facilitate seamless communication between patients and providers.
Ensure Accessibility for Patients
-
Addressing Diverse Patient Populations: Highlight the need for technology that is accessible to diverse patient populations, considering factors such as age, digital literacy, and socio-economic status. Discuss the importance of inclusivity in platform design.
-
Strategies for Overcoming Barriers: Discuss practical strategies for overcoming potential barriers to technology adoption among patients. This may involve providing training resources, offering technical support, and ensuring that the virtual care platform is compatible with a variety of devices.
Implement Robust Training Programs
Train Healthcare Providers
-
Role of Comprehensive Training: Emphasize the critical role of comprehensive training for medical professionals involved in Virtual Care Management. Discuss how thorough training ensures that providers are proficient in utilizing RPM and CCM technologies, maximizing the effectiveness of remote patient monitoring and chronic care management.
-
Ongoing Training for Updates: Highlight the importance of ongoing training programs to keep healthcare providers updated on program enhancements, new features, and best practices. Continuous education enables providers to adapt to evolving technologies and deliver high-quality virtual care.
Educate Patients
-
Resources for Patient Education: Provide a range of resources for educating patients on the use of RPM and CCM technologies. This may include user guides, video tutorials, and interactive materials that empower patients to actively participate in their care.
-
Benefits of Patient Engagement: Explore the potential benefits of patient engagement through education. Discuss how informed and educated patients are more likely to adhere to remote monitoring protocols, leading to improved health outcomes. Encourage healthcare providers to foster a collaborative approach to care by involving patients in their own health management.
Foster Interdisciplinary Collaboration
Facilitate Communication Between Teams
-
Importance of Interdisciplinary Collaboration: Discuss the crucial role of interdisciplinary collaboration in the success of Virtual Care Management programs. Emphasize that effective communication between care teams, including physicians, nurses, specialists, and administrative staff, is vital for delivering comprehensive and coordinated patient care.
-
Strategies for Fostering Communication: Explore strategies for fostering seamless communication between care teams. This may involve implementing communication platforms, regular team meetings, and shared electronic medical records. Encourage open dialogue and the exchange of insights to enhance patient outcomes.
Create a Collaborative Care Culture
-
Benefits of Collaborative Care Culture: Highlight the numerous benefits of cultivating a collaborative care culture within healthcare organizations. Discuss how Virtual Care Management programs contribute to this culture by promoting shared decision-making, care coordination, and a patient-centric approach.
-
Enhanced Coordination Among Professionals: Discuss how VCM programs enhance coordination among healthcare professionals. By breaking down silos and promoting a culture of collaboration, these programs optimize the use of resources, reduce redundancies, and improve the overall quality of care.
Monitor and Evaluate Program Performance
Establish Key Performance Indicators (KPIs)
-
Role of KPIs in Assessing Program Performance: Discuss the pivotal role of Key Performance Indicators (KPIs) in evaluating the success and impact of Virtual Care Management programs. Highlight how KPIs provide measurable metrics that reflect patient outcomes, satisfaction, and operational efficiency.
-
Examples of KPIs: Explore examples of relevant KPIs that align with program objectives. This may include metrics such as patient adherence to remote monitoring, reduction in hospitalizations, improvements in chronic disease management, and overall cost-effectiveness.
Regularly Review and Adjust Strategies
-
Importance of Continuous Improvement: Emphasize the significance of a continuous improvement mindset in the implementation of Virtual Care Management programs. Acknowledge that healthcare landscapes evolve, and regular reviews enable healthcare providers to stay adaptive and responsive to changing needs.
-
Strategies for Ongoing Program Evaluation: Discuss practical strategies for ongoing program evaluation, emphasizing regular reviews of patient feedback, clinical outcomes, and operational processes. Encourage healthcare teams to be proactive in identifying areas for improvement and implementing adjustments accordingly.
Transform Your Patient Care with HealthSnap’s Virtual Care Management Programs
HealthSnap‘s best-in-class Virtual Care Management programs are designed to revolutionize healthcare delivery. With our Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) solutions, you can enhance patient outcomes, streamline workflows, and create a patient-centric care environment. HealthSnap is HIPAA-compliant and HITRUST-certified, ensuring the highest standards of compliance, reliability, and security to support seamless care coordination on a large scale.
To learn more about how HealthSnap’s RPM & CCM programs can transform patient care delivery, call us today at 888-780-1872 (Ext. 3) or click here to schedule a free demo and consultation with a HealthSnap team member.











Leave A Comment
You must be logged in to post a comment.