Over the past few years, the utilization of population health management has witnessed a significant surge due to its ability to drive improved outcomes, cost reduction, and enhanced patient experience. Telehealth and virtual care management programs, particularly Remote Patient Monitoring (RPM) and Chronic Care Management (CCM), have emerged as a vital force behind this trend, empowering healthcare organizations across various locations with a powerful tool to implement effective population health management solutions. In this comprehensive guide, we will delve into the ways RPM and CCM technology and services can support scalable population health programs, benefiting patients, providers, and payors alike.
What is Population Health Management?
Population health management entails a systematic approach to optimize the health of an entire population by monitoring and enhancing the health of individuals within that population. It revolves around scrutinizing healthcare data to identify trends, evaluate risk factors, and take proactive measures to improve care delivery and outcomes.
The scope of population health management encompasses preventive measures such as public education campaigns, screening programs, and early intervention services. By focusing on improving the health of individuals within a population, this systematic approach aids in reducing healthcare costs, enhancing quality of life, and the social environment while mitigating disparities in healthcare access.
The Significance of Population Health Management
Population health management plays a pivotal role in any healthcare system, serving as the foundation for accurate data collection, analysis, and decision-making. As healthcare organizations increasingly strive to transition from a fee-for-service model to value-based care, population health management assumes critical importance in facilitating both payors and providers to promote better health equity and access through efficient resource allocation.
For payors, an effective population health strategy can lead to reduced healthcare costs, increased member engagement, and improved quality of care. By focusing on preventive care and early intervention strategies, providers benefit from enhanced care coordination, enabling them to offer patients a more personalized healthcare experience.
Common Challenges in Managing Population Health
Despite the myriad benefits of population health programs, healthcare organizations encounter various challenges when it comes to managing the health of their populations. These challenges encompass disparate data sources, a lack of standardized metrics, and the necessity to coordinate care across multiple providers and healthcare settings, which can prove to be a practical challenge.
Moreover, some providers may exhibit reluctance in adopting value-based care contracts due to uncertainties regarding organizational readiness and maturity. Securing adequate reimbursement and funding for population health initiatives can also be arduous, given that many payors still operate under a fee-for-service model.
Innovative payors have begun harnessing technology to address these issues and enhance collaboration and communication across the healthcare system.

The Role of Population Health Management Solutions in Care Delivery Today
The utilization of population health management solutions has witnessed steady growth in recent years, and this trend is no coincidence. Designed to improve outcomes by prioritizing specific goals and standards within distinct patient segments, population health management represents an extension of the value-based care standard, which the Centers for Medicare & Medicaid Services (CMS) emphasize. But what exactly is population health management, and how does it assist providers in meeting this new standard of value-based care?
As the name suggests, population health management involves managing specific patient sub-populations as separate groups. By doing so, it empowers providers to treat these populations more efficiently while offering patients more targeted services and interventions.
While population health management originated from the concept of public health, which focuses on addressing social determinants of health (SDOH) to counteract widespread inefficiencies in the healthcare system, it has now evolved into a distinct entity centered on the identification and optimized treatment of specific patient populations.
How does population health management work? By collecting and analyzing high-quality patient data at the individual level and extrapolating these findings to the entire sub-population, population health management solutions can provide a wealth of benefits to all stakeholders involved in the care continuum:
-
Providers can access a higher level of patient data, enabling better decision-making and outcomes. These solutions also present new or improved revenue streams, reduce potentially preventable events, establish the foundation for better clinician-patient relationships, and enhance the overall patient experience.
-
Patients can receive personalized positive behavior coaching and more opportunities to engage with their own care plans. They may also develop a stronger sense of ownership over their treatment goals, driving greater engagement and positive outcomes.
-
Payers can reduce expenses by minimizing readmissions and the likelihood of co-morbidities and other risks, while also decreasing unnecessary interventions and improving CMS reimbursement.
Implemented effectively, population health management fulfills these vital benchmarks, simultaneously achieving the “Triple Aim” of healthcare: enhancing the health of the patient population, elevating the overall quality of care delivery, and curbing the growth of medical costs.
How Population Health Management Solutions Aid in Managing High-Risk Patients
Another significant reason behind the widespread adoption of population health management in the United States healthcare system is its adaptability. Depending on the settings to be employed and the requirements of each population, population health management solutions can be as extensive or as minimal as needed, catering to various budgets and operational workflows.
Chronic care management (CCM) represents one of the most established types of population health management. It is a care management model specifically designed to address patients with two or more chronic conditions. CCM offers healthcare providers a predetermined reimbursement amount for executing specific tasks, including:
-
CPT code 99490: Reimburses the time spent by clinical staff, under the direction of a physician or qualified healthcare provider (QHP), for basic patient coordination services such as arranging follow-up appointments, refilling prescriptions, and requesting and updating medical records.
-
CPT code 99491: Reimburses the time directly spent by a physician or QHP in managing care for patients, covering 30 minutes of time per patient per month (PPPM).
-
CPT codes 99487 and 99489: Cover the same services as 99490 and 99491 but for patients requiring “moderate or high complexity medical decision-making.”
-
HSPCS code G0506: A single-code option encompassing comprehensive assessment and care planning for patients with two or more chronic conditions, separate from the aforementioned codes.
Since the introduction of the first CCM code in 2015, healthcare providers have leveraged this model to achieve population health goals for patients with chronic conditions, which encompass a comprehensive list of high-risk conditions such as stroke, heart disease, diabetes, cancer, chronic obstructive pulmonary disease (COPD), kidney disease, multiple sclerosis, depression, and many others.
It comes as no surprise that these chronic conditions also represent the costliest burden on the U.S. healthcare system. Diabetes alone costs the U.S. healthcare system an estimated $327 billion annually. When combined, stroke and heart disease account for another $216 billion, with cancer at a comparable amount, according to data from the Centers for Disease Control and Prevention (CDC).
These staggering figures have intensified the government’s efforts to reduce healthcare costs. Population health management solutions like CCM are specifically designed to address these challenges effectively, and they heavily rely on telehealth technology such as Remote Patient Monitoring (RPM).
RPM offers a valuable tool for managing high-risk patients by providing continuous monitoring and capturing vital health data remotely. By utilizing RPM, healthcare providers can closely track patients’ health status, detect early warning signs, and intervene promptly to prevent complications. This proactive approach significantly reduces the risk of hospital readmissions, lowers healthcare costs, and enhances patient outcomes.
Furthermore, RPM enables patients to actively participate in their care management. They can easily transmit health data from the comfort of their homes, fostering a sense of empowerment and engagement. RPM also facilitates regular communication between patients and healthcare providers, promoting better care coordination and timely interventions.
The combination of RPM and CCM within a comprehensive population health strategy equips healthcare organizations with the tools necessary to effectively manage high-risk patients and achieve positive health outcomes while optimizing resource utilization.
In a nutshell, population health management is driven by RPM and CCM represents a transformative approach to healthcare delivery. By adopting these solutions, healthcare organizations can harness the power of data, technology, and patient engagement to optimize the health of populations, reduce costs, and improve the overall quality of care. As the healthcare landscape continues to evolve, embracing population health strategies supported by RPM and CCM will be instrumental in shaping a healthier future for individuals and communities alike.

The Empowering Influence of Remote Patient Monitoring and Chronic Care Management on Population Health Outcomes
In the realm of healthcare, Virtual Care Management Programs, like Remote Patient Monitoring programs (RPM), have emerged as revolutionary tools and services that facilitate remote medical care systems and services. Their primary objective is to enhance patient access to healthcare while simultaneously reducing costs and improving operational efficiency. Population health management, a key aspect of healthcare, can be effectively supported by telehealth technology through various modalities, including:
-
Telemedicine: This modality enables healthcare providers to remotely examine, observe, and treat patients through virtual visits. It encompasses medication management, specialist consultations, and Chronic Care Management (CCM).
-
Remote Patient Monitoring (RPM): RPM empowers healthcare providers to remotely monitor patients’ vital signs using cellular-based devices. It facilitates continuous tracking of patient data with connected devices and provides an easily accessible platform for doctors and clinicians to collect and analyze crucial data promptly.
-
Mobile Health (mHealth): Utilizing mobile devices such as smartphones, tablets, and wearables, mHealth delivers healthcare services and grants access to health information.
RPM technology plays a pivotal role in ensuring that doctors and clinical staff possess near real-time patient data for making optimal decisions. By facilitating the regular monitoring and transmission of vital signs and other essential physiological patient information, RPM technology equips healthcare professionals with the necessary insights to prevent escalation or hospitalization, especially for chronic and high-risk patients.
In recent years, the RPM program has evolved beyond being only a part or mere component of care coordination and has emerged as its own care management model. Particularly for managing patients with chronic conditions, RPM reimburses providers for coordinating the setup of RPM devices and the time spent utilizing the collected data. Specific codes have been assigned to different aspects of RPM, such as initial program setup, RPM data collection and analysis, additional clinical time spent with patients, and the collection and interpretation of data.
While care coordination and guidance to the patient are the main focus of Chronic Care Management (CCM), RPM primarily concentrates on establishing the necessary remote devices for at-home care. It also provides reimbursement for staff time dedicated to the usage of these devices, distinct from the administration of the care plan covered by CCM.
The Synergies of Integrating Remote Patient Monitoring Programs with Chronic Care Management
Given their complementary nature, many providers choose to integrate both RPM and CCM into a comprehensive model for managing patients with multiple chronic conditions. This integrated approach improves efficiency, reduces costs, drives population-wide improvements, and maximizes reimbursement.
The benefits of RPM extend to three key aspects of population health program management:
-
Improved Access to Care: RPM eliminates barriers to care, particularly for individuals residing in remote or underserved areas. Virtual care solutions, such as video conferencing, enable patients to connect with healthcare providers without the need for long-distance travel.
-
Increased Patient Engagement: By leveraging RPM, patients can receive medical care from the comfort of their homes and access educational resources to actively participate in their healthcare. RPM also offers reminders and follow-up care, promoting continuity of care and reducing the risk of readmissions.
-
Enhanced Coordination of Care: RPM platforms streamline communication between providers and patients, facilitating information sharing, care plan coordination, and progress tracking. Real-time data and analytics offered by RPM assist payors in identifying care gaps, thereby improving member experience and satisfaction.
Adopting a population health strategy, along with clinical benefits along with incorporating RPM, can foster lifelong changes in health behavior and contribute to overall improvement for both patients and clinics. The increasing emphasis on population health management has resulted in a rise in RPM implementation across hospitals and health systems, with a staggering 88 percent adopting RPM services to enhance population health outcomes, as reported by a consulting firm.
RPM proves to be an optimal solution for chronic disease management by providing healthcare providers in defined public health, public or private sectors, with better data for improved outcomes and increasing patient engagement. Understanding patient behavior patterns is the foundation for promoting behavioral changes.
Population Health Segmentation and the Social Determinants of Health
Population segmentation analysis in relation to emerging public health functions allows healthcare providers to identify specific needs within their patient population, classifying them based on demographics, health status, or general motivation. This stratification aids public health authorities in recognizing social determinants of health (SDOH) within the patient population and identifying common disparities in the community.
According to the National Academy of Medicine, SDOH factors contribute significantly (80-90 percent) to a patient’s health outcomes, surpassing the influence of medical care (10-20 percent). Leveraging SDOH data in conjunction with RPM data enables clinicians to gain a comprehensive understanding of patients’ home lives, facilitating more coordinated and engaged care efforts.
To achieve SDOH interoperability, a framework is required to identify, measure, and activate social risk factors. Tools like artificial intelligence, natural language processing, patient matching and unique patient identifiers, telemedicine, remote patient monitoring and self-care, records management, and algorithms can empower healthcare stakeholders to engage and monitor at-risk individuals across diverse touchpoints within the community.
The Transformative Power of Remote Monitoring and Population Health Data on Patient Segments: Examples
By harnessing the potential of Remote Patient Monitoring and Chronic Care Management programs and leveraging population health data, healthcare providers have been able to enhance patient engagement, improve outcomes, and reduce costs across various patient segments. In this section, we will explore the profound impact of RPM and population health data on specific patient populations, including patients with diabetes, those in rural areas, and individuals aged 65 and older. Furthermore, we will delve into the role of value-based care models in supporting a robust population health strategy and promoting better healthcare outcomes for targeted patient populations.
Patients with Diabetes
RPM has emerged as a powerful tool for enhancing patient engagement and improving outcomes among individuals with diabetes. By providing patients with consistent access to their health data, RPM increases their health literacy and empowers them to adopt proactive behaviors. Moreover, ensuring that patients with diabetes are engaged and comfortable with their care plan significantly improves adherence rates.
A survey conducted across 25 healthcare facilities revealed that RPM programs designed for diabetes management led to a remarkable 38 percent reduction in hospital admissions and a 25 percent decrease in emergency department visits. To launch an effective diabetic population health strategy, clinicians can start by creating a registry of patients with diabetes.
This registry can be compiled using a combination of Electronic Health Records (EHR), telehealth, and RPM data. By monitoring risk factors, lab tests, and medications, clinicians can identify patients who may be at risk of developing diabetes. Once identified, high-risk patients can leverage RPM services to track their vital signs and stay up-to-date with their personalized care plans.
Patients in Rural Areas
Approximately one in five individuals in the United States resides in rural areas, presenting unique challenges when it comes to accessing quality healthcare. Rural populations often experience less favorable health outcomes due to various factors, including increased accidental injuries, higher prevalence of drug and alcohol misuse, and limited access to preventive and emergency care due to transportation barriers.
Moreover, rural areas typically have a higher proportion of aging patients with a higher prevalence of chronic diseases, leading to increased utilization of Medicare and Medicaid services. Tragically, preventable chronic diseases contribute to high mortality rates among rural patients. However, rural hospitals have recognized the potential of remote physiologic monitoring services to address these challenges effectively. The simplicity and geographic accessibility of RPM have enabled rural healthcare providers to overcome barriers such as time, distance, cost, and limited access to quality healthcare services.
Equitable RPM vendors have adopted workflows that consider the specific barriers faced by rural residents. For instance, they may provide cellular-enabled RPM devices, eliminating the need for a strong WiFi connection. By leveraging RPM, healthcare providers in rural areas can bridge the gap in healthcare access and provide timely, high-quality care to their patient populations. The ability to remotely monitor patients’ health data empowers healthcare professionals to intervene proactively, leading to improved health outcomes and reduced healthcare disparities.
Patients Aged 65 and Older
The older adult population is growing rapidly, with individuals aged 65 and older living longer and facing an increasing burden of chronic conditions. This age group requires regular monitoring and management of their chronic illnesses. Fortunately, RPM offers user-friendly technology that enables seniors to age in place comfortably, within the familiar surroundings and physical environment of their homes. Beyond managing chronic conditions, RPM also plays a vital role in ensuring the independence of older adults. With age, the risk of falls increases significantly, but RPM can help prevent, detect, and locate these incidents promptly.
According to the Center for Technology and Aging, greater access to proven remote patient monitoring technologies can lead to safer and more effective monitoring of health and safety among older adults. Falls, in particular, pose a significant threat to the health system for the elderly and result in substantial costs to society. Rapid assistance following a fall has been shown to reduce hospitalization rates by 26 percent and decrease mortality by over 80 percent. By leveraging RPM, healthcare providers gain a timely advantage compared to other preventative tactics, enabling them to intervene promptly and prevent adverse events.
Value-Based Care Models and Population Health Research
Value-based care models have emerged as proactive approaches focused on improving patient outcomes and enhancing the quality of care provided by healthcare providers. These models incentivize healthcare professionals based on the quality of care they deliver, as well as their ability to improve efficiency and effectiveness. This shift from traditional fee-for-service payments to value-based reimbursement models opens up new opportunities for providers to enhance patient care while also improving their financial sustainability.
The Center for Medicare and Medicaid Services (CMS) has been at the forefront of promoting value-based care delivery models, such as the Medicare Shared Savings Program, Next Generation Accountable Care Organization (ACO) model, and the Pioneer ACO model. Private payers have also adopted similar accountable value-based care models. These models reward healthcare providers for their efforts in helping patients lead healthier lives and reducing healthcare costs.
Promoting Value-Based Care for Specific Patient Populations
In line with the goal of promoting value-based care from a population health perspective, CMS introduced Chronic Care Management (CCM) in 2015 and followed it up with Remote Patient Monitoring (RPM) in 2018. These initiatives have transformed the delivery of healthcare services and improved patient outcomes, particularly for individuals with chronic illnesses.
Chronic Care Management is a value-based care initiative that supports overwhelmed healthcare practices in providing comprehensive care for their high-risk and high-cost chronic care patients. It involves the development of a comprehensive care plan, medication adherence support, and coordination between specialists and primary care providers.
Medicare patients with multiple chronic conditions are eligible to participate in CCM programs, and providers receive monthly incentives for each enrolled CCM patient. These incentives, along with fee-for-service payments and shared savings, create a lucrative opportunity for healthcare practices to improve patient care while achieving financial sustainability.
RPM, on the other hand, leverages digital technology and remote devices to capture and transmit patient data, enabling clinicians to assess their patient’s overall condition. Abnormal readings can be quickly detected and used to adjust the trajectory of care. Similar to CCM, CMS provides incentives to healthcare providers for setting up and educating patients, interpreting patient data, and making necessary interventions based on the collected information.
Both CCM and RPM represent a paradigm shift from the quantity-focused approach of traditional fee-for-service reimbursement to a quality-focused approach. Value-based care models have a triple aim: improving patient care, strengthening population health management strategies, and reducing healthcare costs. By implementing CCM and RPM, healthcare providers can achieve these aims by enabling timely and appropriate clinical interventions, optimizing care delivery, gathering necessary clinical data for compliance, significantly reducing costs, and empowering primary care providers to be at the forefront of patient care.
The Bottom Line: Population Health Outcomes
The integration of Remote Patient Monitoring (RPM) and population health research data has the potential to revolutionize patient care across various segments. By leveraging these tools, healthcare providers can enhance patient engagement, improve outcomes, and reduce costs for targeted patient populations. Patients with diabetes can benefit from improved adherence and increased access to their health data, resulting in better disease management.
Individuals residing in rural areas can overcome barriers to healthcare access through the simplicity and geographic accessibility of RPM. The older adult population can enjoy enhanced independence and safety through the use of RPM devices that detect falls and provide timely assistance. Furthermore, value-based care models, such as Chronic Care Management (CCM) and RPM, support a population health strategy by incentivizing healthcare providers to focus on quality care, optimize interventions, gather essential data, and reduce costs.
As healthcare continues to evolve, the integration of Remote Patient Monitoring, population health research data, and value-based care models will play a key role in transforming patient care, improving outcomes, and enhancing the overall health improvement well-being of individuals and communities. By embracing these innovative approaches, healthcare providers can pave the way for a more patient-centered and cost-effective healthcare system.
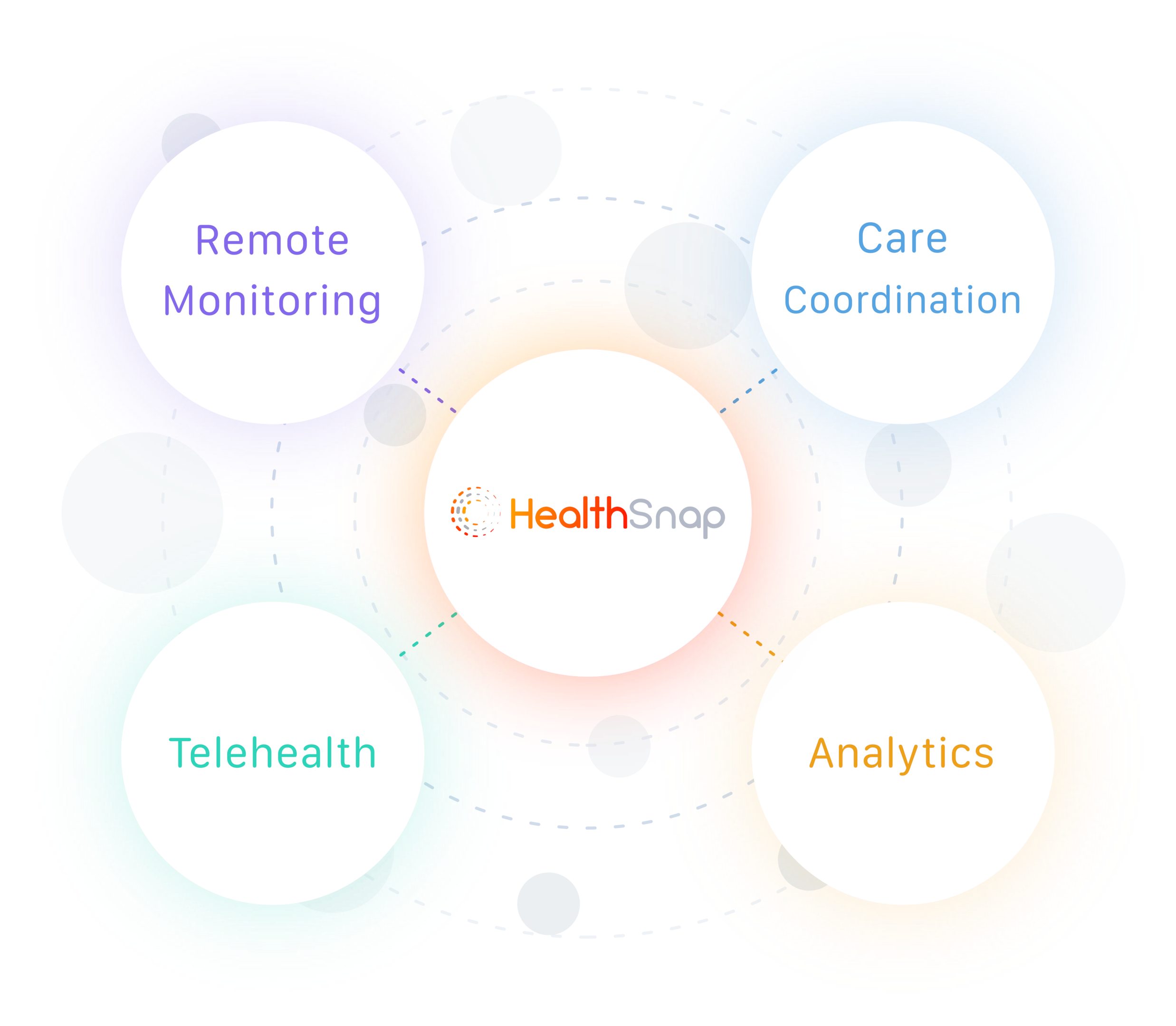
Seeking Effective Virtual Care Management Solutions for Population Health Management? Think HealthSnap!
If you’re looking to harness the power of Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) to achieve critical population health management goals, we are here to assist you. At HealthSnap, we offer comprehensive support and expertise in RPM and CCM. Our team of virtual care management program specialists is ready to guide you through the process. Reach out to us today and connect with an RPM and CCM expert who can provide valuable insights and assistance.
HealthSnap takes pride in unifying your entire care team, enabling better alignment among providers, enhancing management visibility, and offering administrative control. With our integrated Virtual Care Platform, you can experience firsthand how easy it is to drive revenue and improve patient health outcomes. We invite you to schedule a live demo of our platform, where you’ll witness the seamless integration of RPM solutions into your healthcare practices.
To take the first step towards leveraging our Population Health Management solutions, simply book a meeting or give us a call at 888-780-1872 to request a consultation. Our dedicated team is eager to assist you in optimizing your population health strategy, healthcare management processes, and achieving positive patient outcomes.






