The longitudinal health record is a relatively new innovation—most historians credit the American physician Henry Plummer with inventing and implementing the first health record system at the Mayo Clinic in the early twentieth century. Previously, clinical records were written in the private journals of physicians (if they were recorded at all!). This system may have been helpful for acute cases where the physician needed to recall information over a short period of time, but was virtually useless for patients with chronic conditions or for those who required prolonged acute care. Plummer’s elegant solution was to record patient health information on a standardized dossier that could be kept in a centralized location so that it could be amended or appended over time.
Nearly a century later, paper-based medical records have been largely replaced with electronic medical records (EMRs)—relational databases that not only record and store patient data over time but have the potential to identify abnormalities, provide clinical decision support and allow multidisciplinary care teams to coordinate treatment for complex comorbidities. These new systems often fall short of this lofty vision, but as the direct descendent of Plummer’s paper dossier, they remain the best place to store clinical information.
Advances in connected health present new challenges and opportunities for modern EMRs. Wearable and remote health monitors, along with patient surveys and other patient generated health data, provide clinicians with more insight into their patients’ lives than ever before. That data is of little use, though, if it can’t be seamlessly integrated into the clinical workflow and aggregated, displayed and visualized in an insightful, actionable way. EMRs have the potential to one day play a central role in a new kind of data ecosystem that combines connected health data with traditional clinical data, but integrating these new data streams into existing systems is often an expensive and unsustainable task that doesn’t always unlock the full potential of integrated connected health data.
Interoperability Challenges
In 2019, an American living in New York City could easily travel to the most remote parts of the world and access the funds in their primary checking account by going to an ATM. Back at home, though, they might find themselves at an orthopedic specialist waiting for radiology records and images to be faxed, emailed or even couriered from just a few blocks away. Databases for both financial and health records face many of the same challenges—keeping the most sensitive data private and secure while providing measured access to a complex array of stakeholders—but interoperability has been a core strength of finance technology while EMRs continue to struggle even as adoption has skyrocketed.
Connected health represents a particularly difficult challenge for EMR interoperability. Because so many connected health datastreams originate from sources that were originally designed to be consumer-facing, there is little standardization between vendors in the way data is structured, stored and shared. Standards like HL7’s Fast Healthcare Interoperability Resources (FHIR) will eventually provide the framework to address this problem, but FHIR is still in draft status and adoption rates remains low.
Interoperability is possible, though. Apple’s HealthKit framework allows some connected health data to flow from third-party apps and sensors into some EMRs. This functionality is limited to patients with iPhones and still requires substantial provider-side resources to implement and maintain. Custom interfaces can also be developed to link connected health platforms directly with EMRs, but these interfaces are expensive to implement, require all patients to use the same brand of monitors/sensors, and are difficult to maintain (especially given the rapid iteration cycles of consumer technology that require regular updates to custom interfaces).
Thoughtful Clinical Workflow Design is the Best Integration
Perhaps the most compelling argument in favor of integrating connected health data directly into an EMR is that it doesn’t require clinical staff to switch between platforms to view all of a patient’s data. Designing user-centric clinical workflows is critical for any provider, regardless of the technology, and being deliberate and thoughtful in the way connected health is implemented can go a long way towards avoiding disruption and avoid the steep learning curves that often plague EMR-integrated connected health. While using the right technology allows for the potential of success, poorly designed implementation virtually guarantees failure.
Independent platforms are not new to EMRs or clinical workflows—from imaging technology and proprietary lab equipment to implanted pacemakers and analog diagnostic tools, critical pieces of medical technology remain central to clinical care without directly interfacing with EMRs. Coordinating patient data between systems can be challenging, but in many cases the additional flexibility and customization independent of connected health systems outweigh the challenges posed by maintaining and switching between two systems.
Maintaining separate systems also decreases the chances of going into technical debt, a situation where custom development provides added functionality to early adopters but prevents those same early adopters from taking advantage of improvements to standard functionality in the future. In 2019, with the market driving vendors to prioritize improved interoperability, it seems clear that maintaining a separate connected health platform is a good value as the industry works to improve out-of-the-box interoperability and integration.
Conclusion
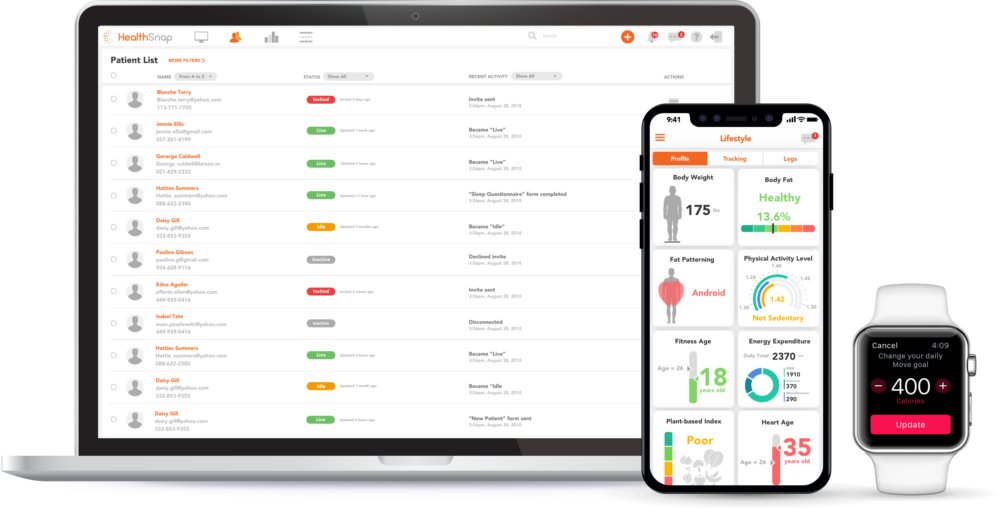
Connected health is coming—patients want it, providers see its potential and payers recognize its value. The convergence of healthcare and consumer technology has not gone smoothly, but that doesn’t mean providers must wait for EMRs and connected health vendors to perfect EMR integration before implementing connected health into their practice. Thoughtful implementation of connected health technology allows patients and providers to utilize this technology now while careful data curation can future-proof systems and allow smooth transitions when the time comes to invest in an integrated system. HealthSnap provides this immediate benefit while safeguarding the future with a turnkey platform that can adapt to any clinical workflow now while at the same time safeguarding data with an eye towards the future.
Sign up for a free trial to easily understand and remotely monitor your patients’ lifestyle health!