As healthcare evolves, integrating technology into patient care becomes increasingly essential. One of the important advancements in this regard is the implementation of Electronic Health Records (EHR), particularly in conjunction with virtual care management programs such as Remote Patient Monitoring (RPM), Chronic Care Management (CCM), and Principal Care Management (PCM).
What is an EHR Integration and why is it important?
Integrating with a healthcare provider’s EHR enables medical records and patient information to be accessed, shared, and managed across various electronic software solutions within healthcare organizations and other digital health platforms. This integration allows different healthcare systems and applications—such as hospital information systems, billing software, telehealth platforms, and virtual care management programs, like Remote Patient Monitoring (RPM) or Chronic Care Management (CCM) —to communicate seamlessly. The goal is to create a unified, interoperable system that provides healthcare providers with comprehensive and up-to-date patient information, ultimately improving the quality of patient care.

An Overview of Virtual Care Management Programs
Virtual care management programs have become the gold standard for managing chronic conditions and facilitating ongoing patient care between office visits. These programs leverage digital technology to improve patient outcomes, enhance access to care, and reduce healthcare costs. Three primary types of virtual care management programs include:
Remote Patient Monitoring
Remote Patient Monitoring utilizes connected health devices and digital technologies to gather and send health information from patients to providers in almost real time. Key features of RPM include:
-
Continuous Monitoring: Patients use connected health devices to track vital signs such as heart rate, blood pressure, glucose levels, or oxygen saturation. This continuous monitoring allows for timely interventions and adjustments in treatment plans.
-
Data Transmission: Collected data is securely sent to healthcare providers, enabling them to assess a patient’s health status without the need for in-person visits.
-
Improved Outcomes: RPM helps in managing chronic diseases, reducing hospital readmissions, and improving overall patient engagement and satisfaction.
Chronic Care Management
Chronic Care Management focuses on coordinating care for patients with multiple chronic conditions. It aims to provide comprehensive support and resources to improve patients’ health outcomes. Key aspects of CCM include:
-
Care Coordination: CCM involves a team-based approach where healthcare providers collaborate to create individualized care plans customized to each patient’s needs.
-
Patient Education: Educating patients about their conditions and self-management strategies is crucial in CCM. This education empowers patients to take an active role in their care.
-
Regular Follow-ups: CCM programs often include regular check-ins via telehealth or phone calls, ensuring ongoing support and monitoring of patients’ conditions.

Principal Care Management
Principal Care Management specifically targets patients with a single chronic condition that requires ongoing care management. Key components of PCM include:
-
Focused Management: PCM emphasizes managing one specific chronic condition, allowing for more tailored interventions and monitoring.
-
Enhanced Access: Patients enrolled in PCM programs have increased access to care through phone calls or telehealth visits, making it easier to receive support and guidance from their healthcare team.
-
Integration with EHR: PCM programs benefit from EHR integration by facilitating seamless communication between healthcare providers and ensuring that patient information is readily available for better decision-making.
The Importance of Setting up an EHR Integration to Scale a Virtual Care Management Program
Implementing an EHR-integrated Virtual Care Management program plays a key role in enhancing the scalability and effectiveness of the programs; particularly across four key areas:
1. Enhanced Data Accessibility
Consolidation of Patient Information
EHR integration consolidates patient data from various sources into a single, unified record. This consolidation includes information from:
-
Different Healthcare Providers: Patient records from multiple providers, including specialists, primary care physicians, and hospitals, can be aggregated into one accessible EHR. This holistic view is essential for coordinating care, especially for patients with complex health conditions.
-
Remote Monitoring Devices: Data from wearable devices and remote monitoring tools can be directly uploaded to the EHR, ensuring that healthcare providers have access to the most current health metrics and trends.
-
Patient-Generated Health Data: Patients can contribute their own data through health apps or patient portals. This patient-generated information adds valuable context to clinical assessments.
Multi-disciplinary Access
EHR integration allows for multi-disciplinary access to patient records, ensuring that:
-
Collaborative Care: Healthcare providers from different specialties can access and share patient information, fostering a team-based approach to care. This collaboration is particularly important in virtual care management, where different providers may be involved in a patient’s treatment.
-
Continuity of Care: Access to a comprehensive patient history helps providers understand previous treatments, allergies, and responses to medications, leading to more informed decision-making and continuity of care.

2. Streamlined Workflows
Reducing Administrative Burdens
EHR integration significantly reduces administrative tasks by automating processes such as:
-
Documentation: Integrated EHR systems can automate data entry and documentation, allowing providers to focus more on patient interactions rather than paperwork.
-
Appointment Scheduling and Reminders: Streamlined scheduling systems integrated with EHR can automatically send reminders to patients for upcoming appointments, reducing no-show rates and improving attendance.
Improving Efficiency in Patient Care
By streamlining workflows, EHR integration enhances efficiency in patient care through:
-
Faster Clinical Decision-Making: With all relevant patient information readily available, providers may be able to make quicker and more accurate clinical decisions, leading to improved outcomes.
-
Optimized Resource Allocation: EHR integration allows healthcare organizations to identify trends in patient demand, enabling better resource allocation and staffing to meet patient needs effectively.
3. Near Real-Time Data Sharing and Communication
Immediate Access to Patient Health Data
EHR integration facilitates near real-time access to patient health data, which is essential for:
-
Timely Interventions: Healthcare providers can monitor patients remotely and respond quickly to any concerning changes in their health status. This immediate access allows for proactive management, reducing the risk of complications.
-
Instant Updates: As patient data is updated in near real-time, providers can stay informed about treatment progress, lab results, and any new health information, ensuring a responsive approach to care.

Facilitating Prompt Interventions
Near real-time data sharing enhances communication among care teams, which supports:
-
Coordinated Care Efforts: Providers can quickly communicate changes in a patient’s condition or treatment plan to all members of the care team, ensuring everyone is on the same page and can act accordingly.
-
Patient Engagement: Near real-time data sharing can also involve patients in their care. For instance, alerts can be sent to patients when their health metrics are outside of acceptable ranges, prompting them to take necessary actions or seek care.
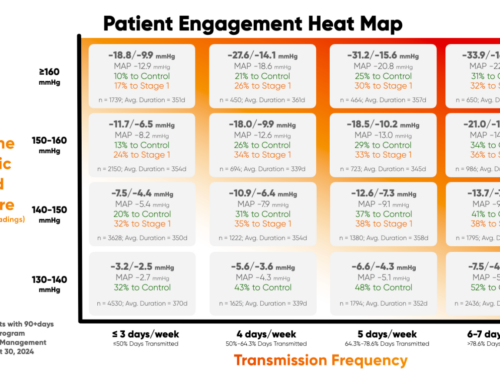
4. Data-Driven Insights
Tracking Patient Outcomes
EHR integration allows for the systematic tracking of patient outcomes over time, which is critical for:
-
Measuring Effectiveness: Providers can analyze the effectiveness of different treatment strategies and make data-informed adjustments to improve patient care.
-
Quality Improvement Initiatives: Healthcare organizations can utilize outcome data to identify areas for improvement, implement changes, and monitor the impact of these initiatives.
Identifying Trends and Patterns
The data collected through EHR integration can be analyzed to identify trends and patterns that inform clinical practice, including:
-
Population Health Management: By analyzing aggregate data, healthcare organizations can leverage population health insights and identify health trends within specific populations. This enables them to design targeted interventions and improve resource allocation strategies.
-
Predictive Analytics: Advanced analytics can predict future healthcare needs and outcomes based on historical data, enabling healthcare providers to prepare for potential challenges and enhance care delivery.
Common EHR Integration Challenges
While an EHR integration streamlines healthcare operations, several challenges must be addressed to ensure a successful implementation.
Interoperability Issues
Compatibility of Different Systems
Interoperability remains a critical challenge for virtual care programs to integrate with EHR systems. Issues may include:
-
Diverse EHR Vendors: Various EHR systems may have different data formats, making it difficult for them to share information seamlessly. This lack of compatibility can hinder the flow of patient data across healthcare settings.
-
Siloed Data: When EHR systems are not interoperable, millions of data points can become siloed within individual organizations, preventing healthcare providers from accessing comprehensive patient histories necessary for effective care.

Solutions to Enhance Interoperability
To address interoperability challenges, healthcare organizations can implement strategies, such as:
-
Adopting Standardized Data Formats: Utilizing widely accepted standards like HL7, FHIR (Fast Healthcare Interoperability Resources), and CCD (Continuity of Care Document) can facilitate better data exchange among different EHR systems.
-
Investing in Interoperability Solutions: Middleware solutions that serve as a bridge between different EHR systems can help improve data exchange and integration. These solutions can aggregate data from multiple sources and present it in a unified format for providers.
Data Security and Compliance
Protecting Personal Health Information (PHI)
The protection of sensitive patient data is paramount in healthcare. EHR integration presents several security challenges, including:
-
Cybersecurity Threats: EHR systems are susceptible to data breaches and cyberattacks, which can compromise sensitive patient information and lead to severe consequences for both patients and healthcare organizations.
-
Access Controls: Ensuring that only authorized personnel have access to PHI is crucial, yet it can be challenging to manage in integrated systems where multiple users may need different levels of access.

Meeting Regulatory Requirements
Healthcare organizations must navigate complex regulatory environments to ensure compliance, including:
-
HIPAA Compliance: The Health Insurance Portability and Accountability Act (HIPAA) sets stringent standards for protecting PHI. EHR systems must be designed to comply with these regulations to avoid penalties.
-
Ongoing Audits and Monitoring: Regular audits and continuous monitoring of EHR systems are essential to ensure compliance with data security standards and regulatory requirements.
Training and Adoption Challenges
Ensuring Staff Proficiency
Successful EHR integration requires that healthcare staff are proficient in using the new systems. Challenges include:
-
Varied Skill Levels: Staff members may have different levels of familiarity with technology, which can affect their ability to utilize the EHR effectively. Comprehensive training programs must cater to these varying skill levels.
-
Continuous Education: EHR systems are constantly evolving, necessitating ongoing training and education to keep staff updated on new features and functionalities.

Overcoming Resistance to Change
Resistance to adopting new technologies is a common challenge in healthcare settings. To overcome this resistance, organizations can:
-
Involve Staff in the Decision-Making Process: Engaging staff in discussions about EHR selection and implementation can foster a sense of ownership and increase buy-in for the new system.
-
Demonstrate Benefits: Clearly communicating the benefits of EHR integration, such as improved patient care and reduced administrative burdens, can help alleviate concerns and motivate staff to embrace the changes.
Best Practices to Successfully Integrate with an Electronic Health Record (EHR)
Successful EHR integrations require careful planning and execution to ensure that healthcare organizations can fully realize the benefits of electronic health records while scaling their virtual care management programs. With the adoption of best practices, EHR integration streamlines virtual care delivery and promotes a win-win situation for all stakeholders.
Selecting the Right EHR System
Prioritizing Interoperability Features
When selecting an EHR system, interoperability should be a top priority. Organizations should:
-
Evaluate Compatibility: Choose EHR systems that have a proven track record of compatibility with other healthcare technologies and standards, such as FHIR and HL7. This ensures that the EHR can easily exchange data with other systems.
-
Assess Data Exchange Capabilities: Look for EHR solutions that offer robust data-sharing features, enabling seamless integration with third-party applications, telehealth platforms, and RPM systems.
Assessing Vendor Support and Services
A reliable vendor can significantly impact the success of EHR integration. Organizations should:
-
Research Vendor Reputation: Investigate the vendor’s history, customer satisfaction ratings, and the success stories of other organizations using their EHR system.
-
Evaluate Support Services: Ensure that the vendor provides comprehensive support, including training, technical assistance, and timely updates to keep the EHR system functioning optimally.
Engaging Stakeholders
Involving Providers and IT Staff
Engaging key stakeholders in the EHR integration process is crucial for its success. Organizations should:
-
Create Cross-Functional Teams: Form teams that include healthcare providers, IT staff, and administrative personnel to facilitate collaboration and communication throughout the integration process.
-
Define Roles and Responsibilities: Clearly outline the roles and responsibilities of each stakeholder involved in the EHR implementation to ensure accountability and effective teamwork.

Gathering Feedback from Patients
Patient feedback is vital for refining EHR systems and ensuring they meet user needs. Organizations should:
-
Conduct Surveys and Focus Groups: Engage patients in discussions about their experiences with EHR systems and gather input on features that would enhance their access to care and engagement with providers.
-
Implement Changes Based on Feedback: Actively incorporate patient feedback into EHR configurations and workflows to improve usability and patient satisfaction.
Ongoing Training and Support
Providing Comprehensive Training Programs
To ensure that staff can effectively use the EHR system, organizations should:
-
Develop Customized Training Sessions: Create training programs that are customized to the needs of different staff roles, focusing on the functionalities and features relevant to each group.
-
Utilize Various Training Formats: Incorporate a mix of training formats, such as in-person workshops, online courses, and hands-on practice, to accommodate different learning styles and preferences.

Establishing Continuous Learning Opportunities
Healthcare technology is constantly evolving, necessitating ongoing education for staff. Organizations can:
-
Offer Regular Refresher Courses: Schedule periodic training sessions to reinforce skills and introduce new features of the electronic health record EHR system, ensuring that staff remains proficient and confident in its use.
-
Encourage Knowledge Sharing: Foster a culture of continuous learning by encouraging staff to share tips, best practices, and insights with each other, creating a supportive environment that promotes collaboration.
Future Trends in Virtual Care Management and EHR Interoperability
As digital health care continues to evolve, the integration of electronic health records with virtual care management programs is expected to undergo significant transformations.
The Use of AI/ML in Health Technology
Artificial intelligence (AI) and machine learning (ML) are poised to revolutionize EHR integration and virtual care management by:
-
Enhancing Data Analysis: AI algorithms can analyze vast amounts of patient data from EHRs to identify patterns and predict health outcomes, enabling healthcare providers to make data-driven decisions and improve patient care.
-
Automating Administrative Tasks: Machine learning can streamline administrative processes, such as coding, billing, and scheduling, reducing the burden on healthcare staff and allowing them to focus more on patient care.
-
Personalizing Treatment Plans: AI-driven insights can facilitate the creation of personalized treatment plans based on individual patient histories and responses to previous interventions.
Telehealth and Remote Monitoring Advancements
Telehealth and Remote Patient Monitoring technologies are rapidly advancing, leading to:
-
Improved Accessibility: Enhanced telehealth platforms will enable patients to connect with healthcare providers easily, facilitating access to care regardless of location. Integration with EHR systems will provide a seamless experience for both patients and providers.
-
Near Real-Time Monitoring: Advances in wearable technology and mobile health applications will allow more powerful continuous monitoring of patients’ health metrics, enabling timely interventions and proactive management of chronic conditions.
-
Data Integration: As telehealth platforms evolve, their integration with EHR systems will become more sophisticated, allowing for real-time data exchange and a comprehensive view of patient health.
The Growing Importance of Patient-Centric Care
As healthcare increasingly shifts towards patient-centered approaches, the importance of EHR integration will continue to rise. Key trends include:
-
Empowered Patients: Patients will have greater access to their health records, enabling them to take an active role in their healthcare decisions. EHR integration will support this trend by providing user-friendly interfaces that allow patients to view and manage their health data easily.
-
Personalized Care Experiences: The integration of EHRs with patient engagement tools will facilitate personalized communication and care experiences tailored to individual patient needs and preferences.
-
Holistic Care Models: EHR integration will support the development of holistic care models that consider patients’ physical, mental, and social health. This approach will enhance care coordination and improve overall health outcomes.

Predictions for EHR Integration Evolution
Looking ahead, several predictions can be made regarding the evolution of EHR integration:
-
Increased Interoperability: The future of EHR integration will see greater emphasis on interoperability among various healthcare systems and platforms, enabling seamless data exchange across different providers and settings.
-
Focus on Data Security and Privacy: As EHR systems become more interconnected, ensuring the security and privacy of patient data will be paramount. Advanced encryption technologies and robust compliance measures will play a crucial role in protecting personal health information (PHI) when an EHR integration is in place.
-
Emergence of Blockchain Technology: Blockchain technology may emerge as a solution for enhancing data security and interoperability in EHR integration. Its decentralized nature could ensure secure data sharing while maintaining patient privacy.
-
Shift to Value-Based Care: The integration of EHR systems will increasingly support value-based care models that focus on patient outcomes rather than volume. EHRs will facilitate the collection and analysis of data needed to evaluate care quality and effectiveness.
Embrace the Future of Healthcare Delivery with HealthSnap
By facilitating near real-time data sharing, HealthSnap enhances the engagement between healthcare professionals and patients, building stronger relationships and enabling informed, data-driven decisions for effective care management.
If you are looking to streamline all your care management programs into one comprehensive platform, HealthSnap’s virtual care management platform offers a robust EHR integration in a scalable and proven approach. Call us at 888-780-1872 or contact us online to schedule a consultation or a demo with our team.











Leave A Comment
You must be logged in to post a comment.