In the world of healthcare, innovative technologies continue to shape the way we approach chronic disease management. One such groundbreaking innovation is Remote Patient Monitoring (RPM), a paradigm shift that empowers both patients and healthcare providers to actively engage in the management of chronic conditions. In this guide, we dive deep into the transformative role of RPM in healthcare, while assessing the accomplishments of HealthSnap’s RPM program in managing hypertension.
The Remote Patient Monitoring Revolution
Remote Patient Monitoring (RPM) represents a revolutionary approach to managing chronic diseases, transcending the constraints of traditional healthcare models. At HealthSnap, a visionary team has harnessed the power of RPM and Chronic Care Management (CCM) to deliver personalized care to patients, no matter where they are located. The year 2023 has brought with it a wealth of data and insights that underscore the transformative impact of RPM in healthcare.
The Collaborative Study
In a new collaborative study titled “Asynchronous Management of Hypertension: The Effectiveness of Remote Patient Monitoring in Mixed Populations,” HealthSnap joined forces with Prisma Health and Virginia Cardiovascular Specialists. This endeavor employed cutting-edge technology, utilizing cellular-enabled blood pressure cuffs that seamlessly transmitted data to an Electronic Health Record (EHR)-integrated Virtual Care Management platform. What further set this program apart was monitoring by licensed clinical staff, who worked closely with patients on remote monitoring data collection, patient health status analysis, and adherence to evidence-based care plans.
Impressive Results
The outcomes of this collaborative study were quite remarkable. A total of 2,761 patients, committed to consistently uploading 30 or more blood pressure readings over a span of at least 90 days, participated. The findings underscored the immense potential of Remote Patient Monitoring as a vital tool in hypertension management across diverse health systems and healthcare organizations.
Let’s look at the numbers:
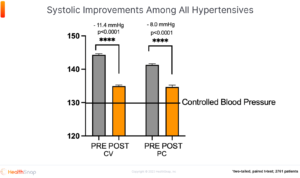
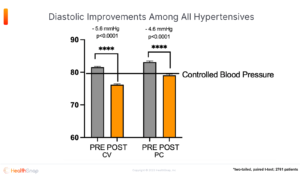
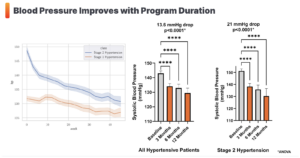
Blood Pressure Improvements: The study revealed substantial improvements in both systolic and diastolic blood pressure, demonstrating the program’s efficacy.
-
In cardiology patients, systolic and diastolic hypertension improved by 11.4 mmHg and 5.6 mmHg, respectively.
-
Primary care patients witnessed reductions of 8.0 mmHg in systolic pressure and 4.6 mmHg in diastolic pressure.
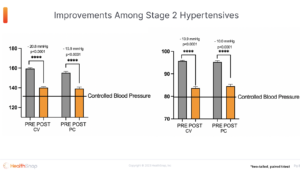
Stage 2 Hypertension: Patients with stage 2 high blood pressure experienced even more significant reductions.
-
Cardiology patients saw a remarkable 20.81 mmHg reduction in systolic pressure and a 13.9 mmHg decrease in diastolic pressure.
-
Primary care patients recorded reductions of 15.9 mmHg in systolic pressure and 10.0 mmHg in diastolic pressure.
Pulse Pressure: Notably, patients with high pulse pressure also benefited from the program, with primary care patients experiencing an average reduction of 6.2 mmHg, and cardiology patients achieving a reduction of 5.8 mmHg.
A Continued Success Story
As we get closer to 2024, HealthSnap’s Remote Patient Monitoring program continues to deliver impactful results, reaffirming its pivotal role in chronic disease management. The success can be attributed to a patient-centered approach, driven by two key factors: engaged healthcare professionals utilizing near real-time data from Remote Patient Monitoring and patient education on evidence-based care plans. This holistic approach combines cutting-edge technology with patients’ own motivation to effect lasting changes, fostering engagement, high patient satisfaction, and promoting evidence-based lifestyle modifications.
The Data
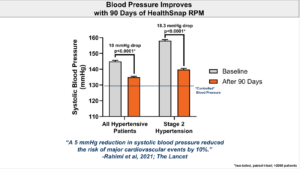
On average, a 10-point reduction in systolic pressure was observed among all hypertensive patients, underscoring the program’s effectiveness (p < 0.0001). The impact was even more pronounced in patients with Stage 2 hypertension, with a remarkable 20-point reduction (p < 0.0001). Importantly, these improvements are not fleeting; they persist over time, suggesting that long-term engagement with HealthSnap’s program yields the most significant benefits.
A Glimpse into Cardiovascular Health
The long-term benefits of reduced systolic pressure are profound, as evidenced by a recent meta-analysis published in Lancet. Each 5-point reduction in systolic pressure could potentially lead to a 10% reduction in cardiovascular events, according to Rahimi et al. (2021). This underscores the potential for HealthSnap’s RPM program to contribute significantly to reducing the burden of cardiovascular disease.
The Power of Care Navigators
One key revelation in HealthSnap’s experience is the key role played by care navigators in amplifying RPM’s efficacy. An in-depth analysis of patient data from one of HealthSnap’s smaller provider groups sheds light on this key aspect. Patients who consistently transmitted data and engaged with the program for at least 90 days witnessed significant improvements:
-
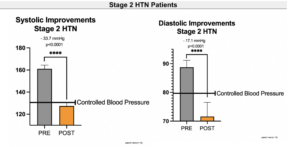
An average systolic pressure improvement of 16.4 mmHg and a diastolic pressure decrease of 8.5 mmHg were recorded (p < 0.0001).
-
For patients with ambulatory or home-based uncontrolled hypertension, the results were nothing short of astonishing. They experienced an average systolic pressure reduction of 26.1 mmHg and a diastolic pressure improvement of 13.1 mmHg (p < 0.0001).
-
The most significant improvements were observed in patients with Stage 2 Hypertension, where systolic pressure decreased by an average of 33.7 mmHg, and diastolic pressure improved by 17.1 mmHg (p < 0.0001).
Looking to the Future
As HealthSnap’s Remote Patient Monitoring program continues to expand its footprint, it holds the promise of bringing remote, concierge-style care to even more patients. This approach ensures that patients remain digitally connected with their healthcare providers and care teams, all from the comfort, safety, and security of their homes. The potential impact on patient outcomes is immense, bridging the gap in healthcare accessibility and equity.
The Role of Cellular-enabled RPM Devices in Hypertension and Cardiovascular Management
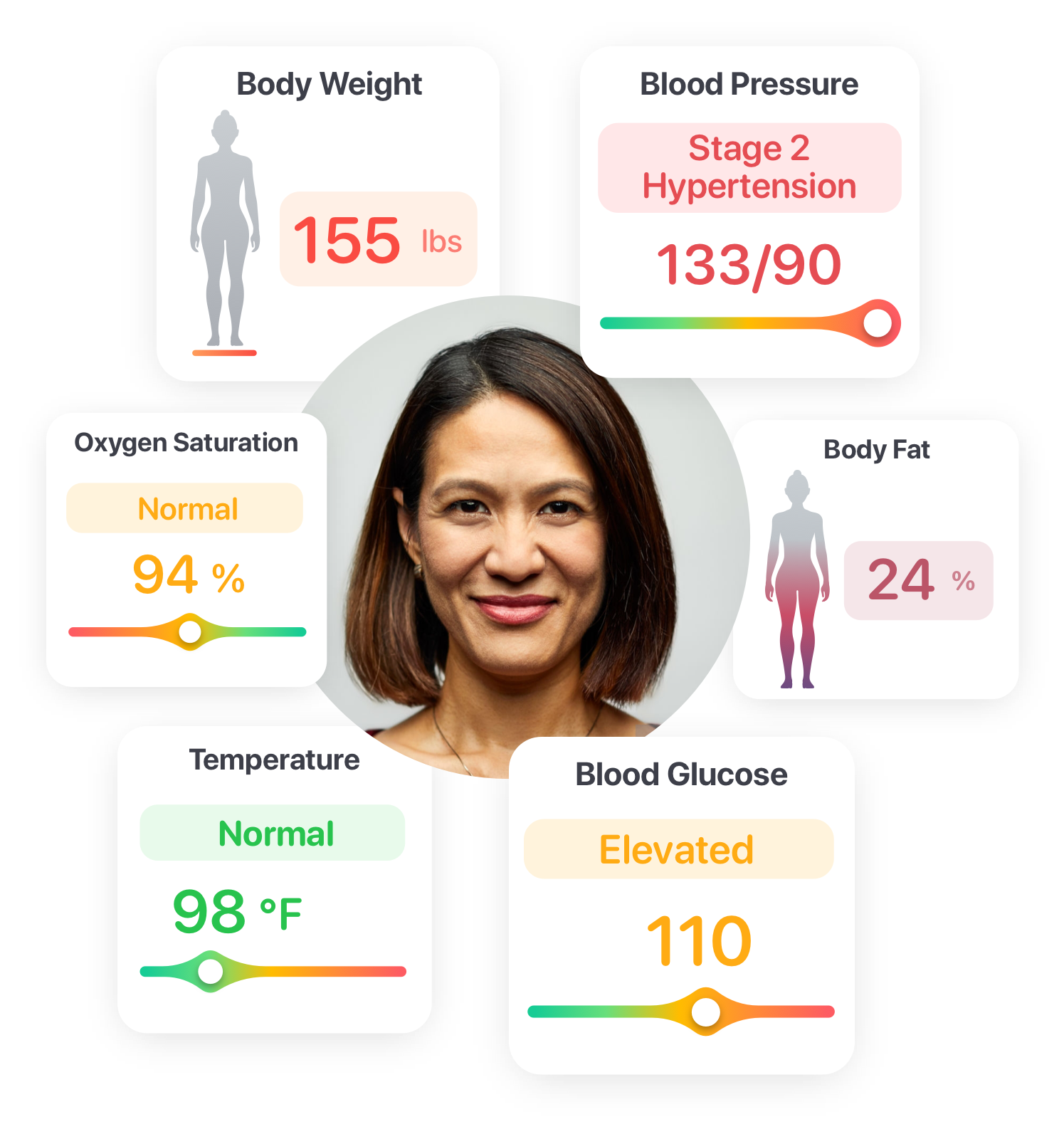
Cellular-enabled RPM devices are specialized healthcare tools that allow patients to monitor critical health metrics, such as blood pressure, from the comfort of their homes. These devices are equipped with cellular connectivity, enabling near real-time transmission of vital data to healthcare providers and monitoring platforms. The adoption of these devices has ushered in a new era of patient-centered care, facilitating timely interventions and more informed treatment decisions.
Hypertension Management: Early Detection of Complications
Hypertension is often referred to as the “silent killer” because it can progress silently without noticeable symptoms until severe complications arise. Cellular-enabled RPM devices support hypertension management by enabling early detection of complications in the following ways:
-
Continuous Blood Pressure Monitoring: RPM devices allow patients to monitor their blood pressure regularly and accurately. Continuous monitoring ensures that even subtle changes in blood pressure are recorded.
-
Near Real-time Data Transmission: These devices transmit blood pressure data in near real time to healthcare providers and monitoring platforms. This allows healthcare teams to closely monitor patients’ blood pressure trends.
-
Alert Mechanisms: RPM devices can be programmed to trigger alerts for extreme blood pressure readings or patterns that suggest complications. This enables rapid response and intervention.
-
Patient Engagement: Patients using RPM devices become more engaged in their healthcare. They are more likely to report unusual symptoms or seek medical attention if they notice significant changes in their blood pressure readings.
-
Customized Alerts: Healthcare providers can set customized alert thresholds based on individual patient profiles. This ensures that interventions are tailored to each patient’s specific needs.
-
Preventive Measures: Early detection through RPM devices allows healthcare providers to implement preventive measures promptly. Adjustments to medication regimens, lifestyle recommendations, and referrals to specialists can be made to address complications.
Hypertension Management: Data-Driven Lifestyle Changes
Lifestyle factors, including diet, physical activity, stress management, and smoking cessation, play a significant role in hypertension management. Examples of data-driven lifestyle changes include:
-
Dietary Modifications: Patients can use RPM data to identify how their blood pressure responds to changes in dietary habits, such as reducing sodium intake or increasing potassium-rich foods. They can adjust their diets based on these insights.
-
Exercise Routines: Patients can track the impact of physical activity on their blood pressure. They can use this data to develop exercise routines that are effective in lowering blood pressure.
-
Stress Management: RPM data can highlight periods of increased stress and their effect on blood pressure. Patients can employ stress reduction techniques, such as mindfulness or meditation, and monitor their effectiveness through RPM.
-
Medication Adherence: Patients can link their medication adherence to blood pressure changes. This reinforces the importance of taking prescribed medications regularly.
-
Motivation and Accountability: Patients using Remote Patient Monitoring devices are more likely to stay motivated and accountable for their health. Knowing that their healthcare team is monitoring their progress encourages adherence to lifestyle changes.
Cardiovascular Management: Post-operative Care
Cardiovascular procedures, such as heart surgeries, angioplasties, and stent placements, are complex and can have a profound impact on a patient’s overall health. After undergoing these procedures, patients require attentive post-operative care to ensure a smooth recovery and to minimize the risk of complications. Examples of post-operative care with RPM devices include:
-
Heart Surgery Recovery: After cardiac surgery, RPM devices can continuously monitor a patient’s heart rate, blood pressure, and oxygen levels. Any signs of arrhythmias or fluctuations in vital signs can be promptly addressed.
-
Angioplasty and Stent Placement: Patients who have undergone angioplasty or stent placement procedures can benefit from RPM devices that monitor for any signs of restenosis or thrombosis in the treated arteries.
-
Heart Failure Management: Patients with heart failure may require RPM devices to monitor fluid retention, assess for worsening symptoms, and adjust diuretic medications as needed.
-
Rehabilitation: RPM devices can support post-operative cardiac rehabilitation programs by monitoring patients’ exercise tolerance, heart rate response to physical activity, and blood pressure during exercise sessions.
Cardiovascular Management: Heart Failure Management
Managing heart failure involves optimizing medications, monitoring fluid levels, and making lifestyle modifications. This is a dynamic process that requires ongoing assessment and adjustments to treatment plans. Examples of heart failure management with RPM devices include:
-
Optimizing Medication Regimens: RPM devices can monitor patients’ vital signs and symptoms, enabling healthcare providers to adjust medication dosages or add new medications as needed to control heart failure symptoms.
-
Detecting Fluid Retention: Daily weight measurements using RPM devices can help detect fluid retention, a common symptom of heart failure. Early intervention with diuretics can prevent exacerbation of symptoms.
-
Exercise Monitoring: Patients can use RPM devices to monitor their exercise tolerance and heart rate response during physical activity. This information can guide safe and effective exercise routines for heart failure patients.
-
Symptom Reporting: RPM devices often include features that allow patients to report symptoms such as shortness of breath, swelling, or chest pain. Healthcare providers can review these reports and adjust treatment plans accordingly.
Cardiovascular Management: Prevention of Cardiovascular Events
Examples of cardiovascular event prevention with Remote Patient Monitoring devices include:
-
Hypertension Control: RPM devices monitor blood pressure continuously and alert healthcare providers to elevated readings. This early intervention can prevent hypertension-related events like strokes and heart attacks.
-
Cholesterol Management: Patients with high cholesterol levels can use RPM devices to track their progress while on cholesterol-lowering medications or dietary interventions.
-
Diabetes Management: RPM devices can help individuals with diabetes monitor their blood glucose levels and adhere to medication and dietary recommendations, reducing the risk of cardiovascular events.
-
Exercise and Diet: Patients can monitor their exercise routines and dietary habits using RPM devices. This information allows healthcare providers to make recommendations for heart-healthy lifestyle modifications.
Optimize Chronic Condition Management with HealthSnap’s Virtual Care Platform
HealthSnap’s Virtual Care Management Platform is revolutionizing the management of chronic diseases by offering continuous, proactive, and remote patient care to high-risk chronic populations. HealthSnap is HIPAA-compliant and HITRUST-certified, ensuring the highest standards of compliance, reliability, and security to support seamless care coordination on a large scale.
To learn more about HealthSnap’s virtual care management programs and to schedule a free demo, call us today at 888-780-1872 (Ext. 3) or click here to set up a consultation with our experts.











