By Samson Magid, Chase Preston, & Wesley Smith, Ph.D.
Remote Patient Monitoring (RPM) Is Medicinal & Highly Significant
It feels like yesterday when we recall the tense anticipation as our Mac computer pinwheeled while we were analyzing the results from our Remote Patient Monitoring (RPM) program. This was the first time we had a robust sample size that allowed us to assess if our vision and mission of improving patient outcomes was becoming a reality. Since hypertension is one of our most common use cases, we were testing the change in systolic pressure from enrollment to the most recent measurements in patients who had been on the program for at least 90 days. This analysis would help us to confirm that as a company, we were truly making a difference.
Our system was built on existing evidence, suggesting that RPM works best when it integrates seamlessly with physicians, allowing data to inform clinical decision-making in a streamlined and proactive manner. The care navigation was designed to establish a meaningful bond with patients, aiming to enhance their self-efficacy and health literacy around their condition. We believed the approach we were taking was evidence-based and should be making a difference, but we wouldn’t know for sure until the pinwheel on our Mac came to a stop and yielded our first statistical p-value.

Akin to a statistical drumroll, the test revealed that pre-post, systolic blood pressure (SBP) improvements were highly statistically significant at the p < 0.0001 level. We had to set our coffee aside and double-check the data being analyzed, the standard error, and everything else before repeating the analysis as the results were even better than we had hoped.
You see, HealthSnap has its roots in academia, a world where we aim for p < 0.05. It is a ‘line in the sand,’ a defining boundary in the realm of data science and research that serves as a threshold, distinguishing significant findings from those that might just be an artifact of chance. P < 0.05 indicates there’s less than a 5 in 100 probability that the observed phenomenon is coincidental. In contrast, a p < 0.0001 suggested there was a better than 1 in 10,000 chance that the improvement in blood pressure was real – not random.
For those whose memories of college statistics courses have faded, it’s crucial to remember that high statistical significance – particularly in studies with large sample sizes – doesn’t automatically equate to clinical significance of comparable magnitude. In simpler terms, a finding can be statistically significant yet yield relatively modest real-world results. For instance, a 1.0 mmHg improvement in blood pressure might be statistically significant, but from a clinical standpoint, it’s not exactly groundbreaking. But, that wasn’t the case here, our test revealed an 18-point improvement in systolic pressure; which was clinically outstanding.

As a matter of perspective – there is good evidence to suggest that a 5-point reduction in systolic pressure reduces cardiovascular events by 10%. Moreover, large, multicenter, randomized controlled drug trials, such as the Heart Outcomes Prevention Evaluation (HOPE), showed that a common class of blood pressure medication in 9000 patients lowered blood pressure systolic by just 2.4 mm Hg and diastolic by 1.0 mm Hg, and lead to significantly reduced rates of death, myocardial infarction, and stroke among a broad range of high-risk patients. What we were seeing from our RPM system was many times more in the way of blood pressure improvement – so we were seeing a powerful and medicinal effect of the system, and most of these patients were already on blood pressure-lowering medication. This was astonishing.
The clinical outcomes certainly seemed impressive but we had to temper our enthusiasm. This was not a randomized, double-blind, controlled trial. This was uncontrolled, de-identified, retrospective, aggregate health data. We needed to really consider what could be going on. HealthSnap patients are sent a blood pressure cuff that has a cellular chip and seamlessly sends a Wi-Fi signal to the portal, which integrates directly with the EHR. The cuffs are FDA-approved and thoroughly tested for accuracy. But maybe the first versus the last measurement isn’t the most accurate way to compare the readings. We want to truly understand the data here, and analyze and interpret it as ethically as possible before presenting this to the world.
One thing we clearly had to consider was the learning effect. For example, maybe the first time the patient takes the device out of the box and fumbles around with it, the blood pressure reading is artificially high. It could be taken inaccurately, or after a cup of coffee, or late after a stressful day. So, instead, we decided to compare the average of the first 7 days of data transmission to the average of the last 7 days, to account for the acclimatization period and for daily variability. We felt this could provide us with a more authentic comparison between readings from enrollment to 90 days later.
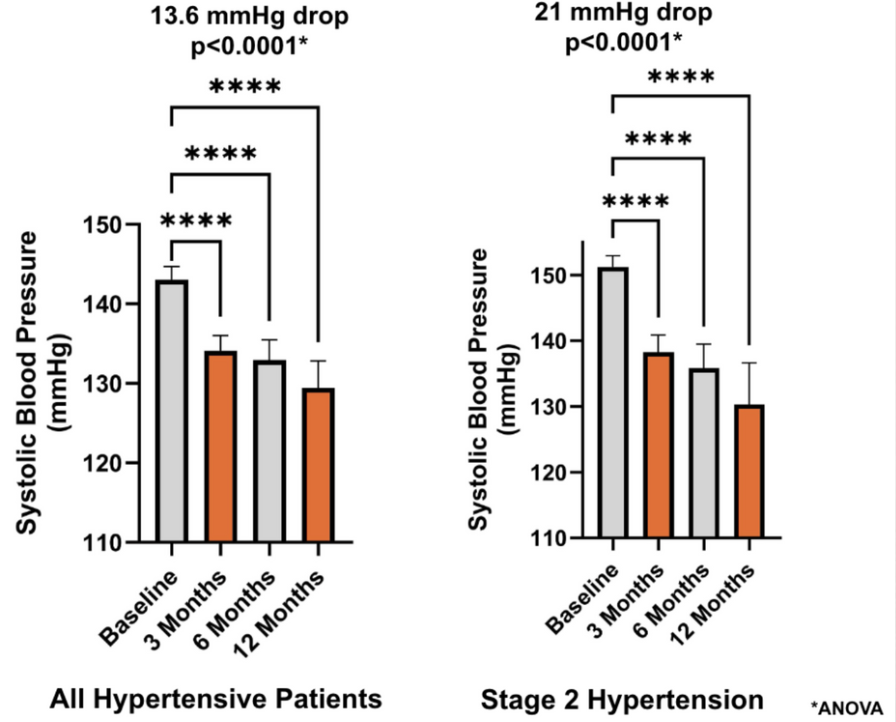
Once again, in this re-analysis, highly significant, clinically meaningful results (over 17-point improvement in systolic pressure and p < 0.0001) were found. Now, we were even more convinced and excited, not just for the company, but for the digital age of healthcare as a whole. Remote care will need to increase in the future and we’ve never been more convinced. Currently, across multiple portals and thousands of patients, we see hypertensive patients averaging a greater than 13 point improvement in SBP and 6.9 points in DBP after 90 days (p < 0.0001), and an over 20 point improvement in SBP among patients with stage 2 levels (SBP ≥140 mmHg). And these results increase in magnitude and significance over time.
RPM is More Than Just Self-Monitoring
Before sharing this data with healthcare providers and health systems, we first analyze these findings using a cynic’s lens. If being pitched the importance and efficacy of using RPM to boost revenue and improve patient care, perhaps providers would ponder if the system THIS company (HealthSnap) uses is really necessary? If home monitoring is effective, and most of our patients already have a BP cuff at home, why not just ask them to take the measurements regularly and share them with us during appointments? Instead of clinical staff reaching out and performing regular care navigation, why don’t we just send some educational material and health counseling?
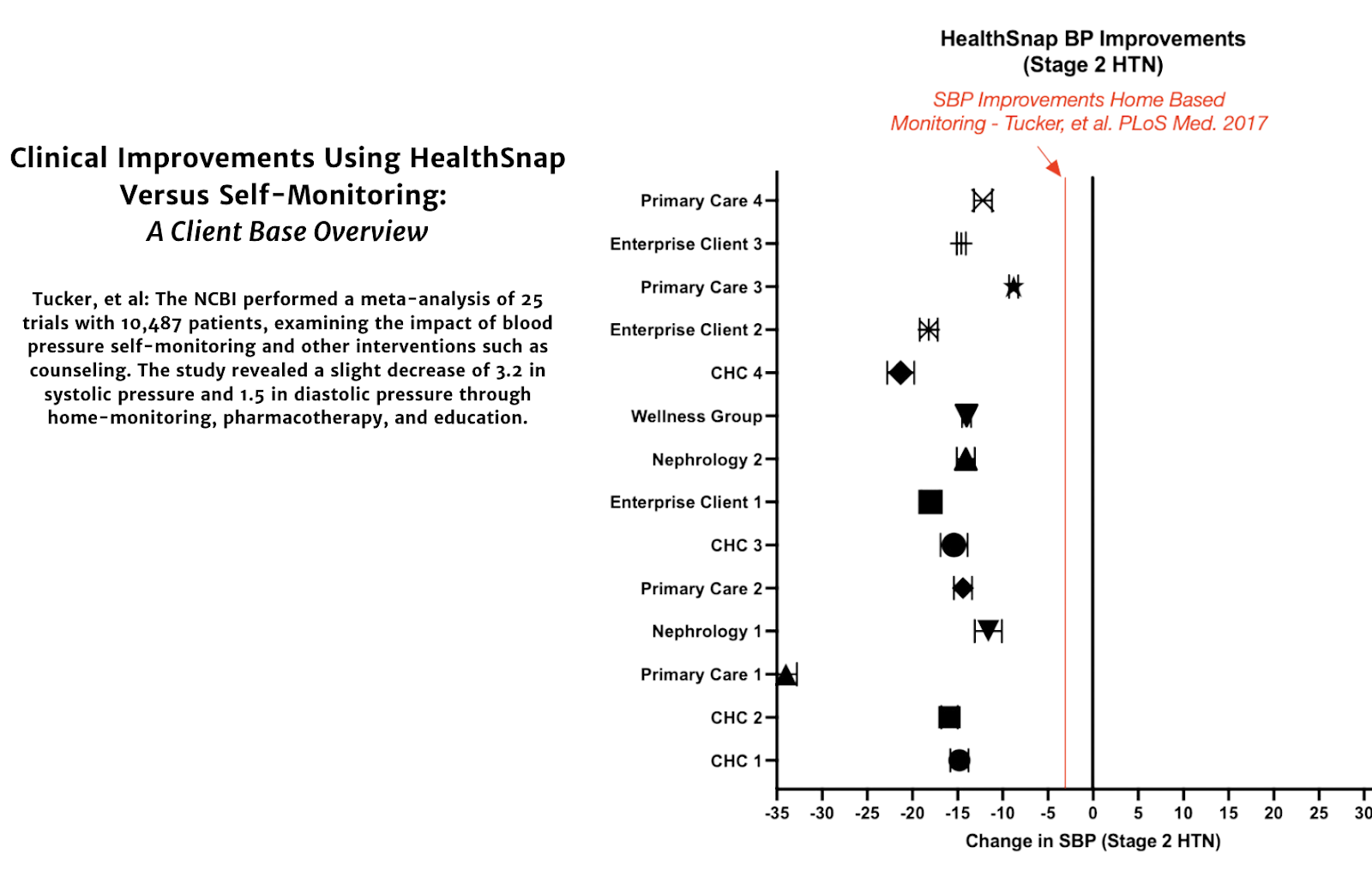
Well, doing just that, a meta-analysis by Tucker et al included data from 25 trials and over 7,000 patients, to see the effectiveness of self-monitoring blood pressure in hypertensive patients. The research found that self-monitoring alone could not significantly reduce blood pressure or improve control. But, when combined with other interventions such as medication adjustments, education, or lifestyle counseling, self-monitoring resulted in a significant, 3.2 mmHg reduction in systolic blood pressure at 12 months. But this was still much lower than what we’re witnessing with Remote Patient Monitoring. It seems clear, that RPM works much better, as physicians using our system were seeing 300-1000% greater improvement across our even larger sample of patients than used in this meta-analysis.
Especially as we consider that in most cases this system is free to patients – as sales-pitchy and icky cliché as this statement seems, we’re going to state it emphatically – we cannot understand why any clinician would NOT use RPM to manage hypertension. And this, essentially, is the data talking.
Masked Uncontrolled Hypertension Is Real
Home monitoring is usually considered a great way to get patients’ real-life blood pressure without the white coat phenomenon often seen in the office. A white coat effect, where a person’s anxiety about being evaluated in the medical office setting artificially raises blood pressure, is suspected to occur about 15-30% of the time. And yes, while remote monitoring from the comfort of a patient’s home will likely combat the white coat artifact in the in-office measurement, our data suggests there is a reverse white coat effect that is potentially even more common and another strong reason why Remote Patient Monitoring for blood pressure should be the standard of care.
Masked uncontrolled hypertension (M.U.C.H.) occurs when a patient has artificially controlled blood pressure in the office, but their home, ambulatory blood pressure is uncontrolled. Simply put, it’s much higher at home than in the medical setting. Patients prescribed RPM are often being treated with medication to control their BP, and the in-office measurement suggests the patient is responding to treatment and their numbers look good. In these “controlled” patients, RPM is prescribed to ensure the BP management is maintained over time; but we’re seeing more than half of these patients, in their home-ambulatory environment, are often uncontrolled upon enrollment (≥130 SBP or ≥80 DBP).
Similar to the white coat, if MUCH is this common, it becomes very difficult to be sure if your patient is responding to treatment appropriately by relying on in-office readings alone. We, and our healthcare clients, have been intrigued and surprised to see the extent of M.U.C.H. among patients, and it even further demonstrates that RPM of BP for patients with hypertension should be the standard of care.

Bridges Gaps in Healthcare Equity & Access
Finally, another no-brainer for the implementation of RPM is to address the concerning gaps in healthcare equity and access among our patients, particularly among those in socioeconomically disadvantaged urban and rural communities. Indeed, an under-appreciated risk factor for disease is a person’s zip code. But an obvious solution to bring a concierge-level of proactive care to these patients is through digital advances, perhaps most notably – Remote Patient Monitoring.
HealthSnap dropships a free, cellular-enabled RPM device to the patient, and clinical outcomes among our Federally Qualified Health Systems and Rural Community center patients have been incredible. And the patients USE the system. In over thousands of patients in more than 20 of these centers in our portal, the average patient is transmitting data more than 60% of the days in the month, and the blood pressure improvements among patients with ≥140/≥90 average over 18 points systolic and a startling more than 11 points diastolic (p < 0.0001).
With diastolic pressures improving that much, it is important to note that there is also an impressive decrease in pulse pressure of nearly 7 points (p < 0.0001) and Mean Arterial Pressure improves by 11.5% (p < 0.0001). Seeing improvements like this among any patient population is shocking, but especially rewarding in this demographic, where this remote style of care can be implemented among a population that struggles with access and frequently misses regular office visits.

In Summary
The efficacy of Remote Patient Monitoring is information that everyone in healthcare should know. The revelation that RPM is revolutionizing hypertension management is not hyperbolic – as there is a better than 1 in 10,000 chance that (p < 0.0001) we’re witnessing ground-breaking improvements in blood pressure across thousands of RPM users. These effects far surpass the effects of self-monitoring alone, highlighting the efficacy of the system as a whole. Furthermore, RPM is unmasking the prevalence of Masked Uncontrolled Hypertension (M.U.C.H.), a condition where blood pressure readings are artificially controlled in the office but uncontrolled at home; this further underscores its necessity as a standard of care in managing hypertension.
Perhaps most exciting of all, for those of us charged with the mission and vision of helping the most people and transforming the healthcare landscape, RPM can address healthcare equity and access gaps, particularly in disadvantaged urban and rural communities. With a cost-free, cellular-enabled RPM device, patients are producing impressive clinical outcomes, actively using the system and transmitting data frequently. Such remote care is especially beneficial for those who often struggle with access and miss regular office visits.
Anyone witnessing these outcomes firsthand will strongly advocate for the use of Remote Patient Monitoring in managing hypertension, recognizing that this approach can mark a significant stride forward in the implementation of digital-age healthcare. This not only aligns with the mission of healthcare providers and companies alike but also promises a brighter, healthier future for patients in the United States and across the world as it expands and these improvements become more well-known.






