Hypertension, commonly known as high blood pressure, is a chronic condition that affects millions of people worldwide and is a major risk factor for cardiovascular diseases, stroke, and kidney failure. Traditional management of hypertension often relies on periodic visits to healthcare providers and self-reported blood pressure readings. With that said, the advent of Virtual Care Management programs, which include Remote Patient Monitoring and Chronic Care Management, has revolutionized how hypertension is managed. These programs leverage technology to provide continuous monitoring and personalized care, leading to improved health outcomes.
Prevalence of Hypertension and its Management Challenges
Hypertension affects over 1.28 billion people globally, with nearly half of these individuals unaware of their condition. The challenge in managing hypertension lies in its often asymptomatic nature, making regular monitoring and timely interventions essential. Traditional in-clinic measurements can be infrequent, leading to gaps in data that may prevent optimal management. Moreover, patients’ adherence to medication and lifestyle changes is often inconsistent, further complicating management.
The Role of Virtual Care Management Programs in Managing Hypertension
Virtual Care Management (VCM) programs encompass various digital health tools designed to enhance patient care beyond the traditional healthcare setting. Remote Patient Monitoring (RPM) and Chronic Care Management (CCM) are two key components of VCM that have shown significant promise in managing chronic conditions like hypertension.
Remote Patient Monitoring
Remote Patient Monitoring refers to the use of digital technology to collect health data from patients outside of traditional healthcare settings. This data, which can include blood pressure readings, heart rate, and other vital signs, is transmitted to healthcare providers in near real-time, enabling timely interventions and personalized care adjustments. For hypertension, RPM often involves the use of cellular-enabled home blood pressure monitor that automatically sends readings to a healthcare provider’s electronic health record (EHR) system.

Chronic Care Management
Chronic Care Management refers to the coordinated care and management of patients with chronic conditions, such as hypertension, over an extended period. Under CCM programs, patients receive regular check-ins, medication management, lifestyle advice, and ongoing monitoring from a dedicated care team. This approach is designed to ensure that patients adhere to their treatment plans, address any emerging issues promptly, and maintain a better quality of life.
The Centers for Medicare & Medicaid Services (CMS) have recognized the value of CCM and provide reimbursement for services aimed at patients with multiple chronic conditions, including hypertension. These services typically involve 20 minutes or more of non-face-to-face care coordination per month.
How RPM Improves Hypertension Outcomes
Enhanced Blood Pressure Control
One of the most significant benefits of RPM in hypertension management is improved blood pressure control. A study published in the Journal of Clinical Hypertension found that patients enrolled in remote blood pressure monitoring programs experienced a substantial reduction in both systolic and diastolic blood pressure compared to those receiving standard care. The continuous monitoring allows for more accurate and frequent assessments, leading to timely adjustments in treatment plans.
Early Detection and Intervention
RPM facilitates early detection of abnormal fluctuations in the patient’s blood pressure, enabling healthcare providers to intervene before the condition worsens. For example, a patient whose blood pressure readings consistently trend upward can receive a timely consultation to adjust medication or lifestyle recommendations, potentially preventing a hypertensive crisis.
Increased Patient Engagement and Adherence
RPM encourages patients to take an active role in managing their condition. The near real-time blood pressure measurement feedback provided by RPM systems can motivate patients to adhere to prescribed treatment plans, as they can see the direct impact of their actions on their health metrics. Studies have shown that increased patient engagement through RPM leads to better adherence to antihypertensive medications and lifestyle modifications.
Reduction in Healthcare Utilization
By improving blood pressure control and enabling early interventions, RPM can reduce the need for emergency room visits and hospitalizations related to hypertension. The ability to monitor blood pressure remotely not only improves patient outcomes but also leads to significant cost savings for healthcare systems. A report published in Science Direct highlighted that RPM programs for hypertension could reduce healthcare costs by preventing complications associated with poorly controlled blood pressure.
Improvement in Long-Term Outcomes
The long-term benefits of measuring blood pressure using RPM are profound. Continuous monitoring helps in maintaining optimal blood pressure levels over extended periods, thereby reducing the risk of long-term complications such as cardiovascular disease, kidney damage, and stroke. Pertaining to this, RPM has been associated with better patient outcomes in high-risk populations, including those with resistant hypertension or multiple comorbidities.

The Future of RPM in Hypertension Management
RPM is expected to play an increasingly important role in home blood pressure monitoring and hypertension management. Advances in artificial intelligence (AI) and machine learning may further enhance RPM systems by enabling predictive analytics of blood pressure measurements and personalized treatment recommendations. Moreover, broader adoption of telemedicine and changes in reimbursement policies could make Remote Patient Monitoring programs more accessible to a wider range of patients.
How CCM Improves Hypertension Outcomes
Enhanced Patient Engagement and Adherence
One of the primary benefits of CCM is increased patient engagement. Regular communication with healthcare providers helps keep patients accountable for their treatment plans, including medication adherence, diet, and exercise. Studies have shown that patients enrolled in CCM programs are more likely to adhere to their prescribed antihypertensive medications, leading to better blood pressure control and reduced risks of complications.
Personalized Care Plans
CCM allows for the development of personalized care plans matching to the specific needs of each patient. These plans consider factors such as age, comorbidities, lifestyle, and socioeconomic status, providing a more holistic approach to hypertension management. This personalization leads to more effective treatment strategies and better patient outcomes.
Continuous Monitoring and Early Intervention
Through regular monitoring and communication, CCM enables healthcare providers to detect early signs of deteriorating blood pressure control. This proactive approach allows for timely interventions, such as adjusting medications or providing additional lifestyle counseling, which can prevent the condition from worsening. Research has demonstrated that patients under CCM programs have fewer emergency room visits and hospitalizations related to hypertension.
Improvement in Long-Term Outcomes
The long-term impact of CCM on hypertension is significant. By maintaining consistent blood pressure control, patients are less likely to develop severe cardiovascular complications, such as heart attacks or strokes. Additionally, CCM has been associated with a reduction in all-cause mortality among hypertensive patients, highlighting its role in extending patients’ lives and improving their overall quality of life.

Reduction in Healthcare Costs
By preventing complications and reducing the need for acute care, CCM programs can lead to substantial cost savings for both patients and healthcare systems. The reduction in hospital admissions, emergency room visits, and the need for expensive interventions translates to lower overall healthcare expenditures. In the long run, the investment in CCM programs is offset by these savings, making it a cost-effective approach to hypertension management.
The Future of CCM in Hypertension Management
CCM will likely play an increasingly central role in the management of hypertension and other chronic conditions. Advances in digital health, including telemedicine and remote monitoring, will further enhance CCM’s capabilities, allowing for even more personalized and proactive care. Moreover, as more data becomes available on the long-term benefits of CCM, we can expect broader adoption and integration of these programs into standard care practices.
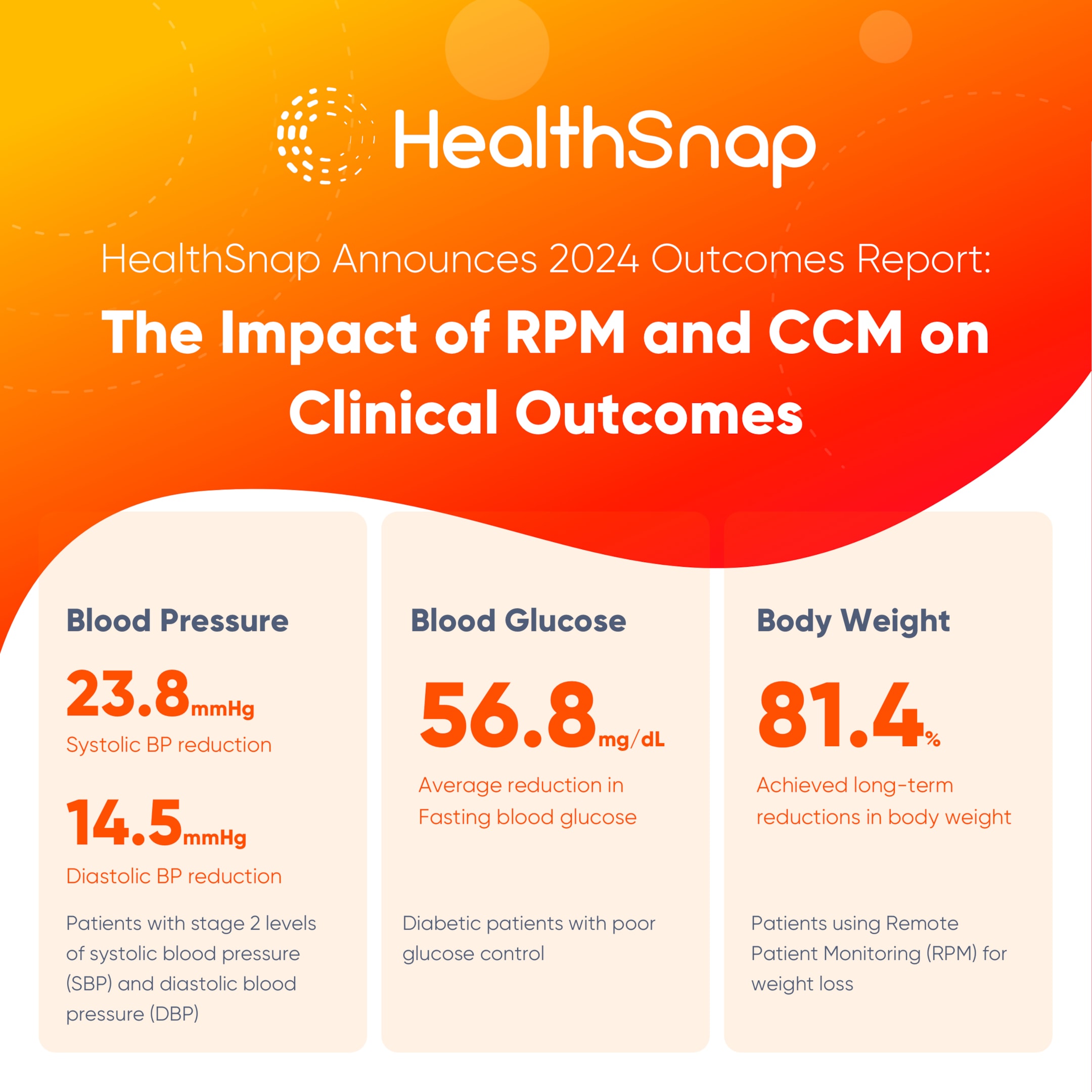
HealthSnap 2024 Healthcare Outcomes Report
HealthSnap is a leading Virtual Care Management platform that assists healthcare organizations in improving patient outcomes, reducing hospital visits, and increasing revenue through programs like Remote Patient Monitoring, Chronic Care Management, and Principal Care Management. HealthSnap works with over 150 healthcare systems and provider organizations in 33 states and has remotely monitored and managed the health of more than 100,000 patients.
Key Results & Measuring Success
To determine how effective HealthSnap’s RPM and CCM programs are, the company analyzed data from 41,940 patients who were in the program for at least 90 days and regularly transmitted their health data. The analysis involved comparing each patient’s initial seven data transmissions (baseline) with the average of their most recent seven transmissions. The results showed significant improvements in blood pressure:
-
Systolic Blood Pressure (SBP): Decreased by 23.8 mmHg.
-
Diastolic Blood Pressure (DBP): Decreased by 14.5 mmHg.
These improvements were particularly notable in patients with stage 2 hypertension, which is a more severe form of high blood pressure.
Impact on Chronic Disease Outcomes
HealthSnap’s RPM and CCM programs have had significant positive effects on overall health, including:
-
Reduced Chronic Disease Risks: Lower blood pressure and blood glucose levels reduce the risk of heart disease, stroke, and complications from diabetes.
-
Fewer Hospital Visits: Better-managed health conditions lead to fewer emergency room visits and hospitalizations.
-
Protection of Eyes and Kidneys: Improved blood pressure helps prevent damage to the eyes and kidneys.
Economic Benefits
Better health management through HealthSnap’s programs translates to significant savings in healthcare costs. By reducing the need for medical interventions, hospital stays, and emergency care, patients and healthcare systems experience economic stability. Decreased medical expenses ease the financial burden on both patients and the healthcare system.
Enhancing Healthcare Access and Equity
HealthSnap’s virtual care management programs help bridge gaps in healthcare access and equity. Patients can receive consistent care regardless of their location, making healthcare more accessible to underserved populations. This helps level the playing field for all patients by providing equal opportunities to manage and improve their health, even between in-office visits.
Methodology for RPM of Blood Pressure
Aggregate, retrospective, de-identified health data was exported from the HealthSnap data portal to evaluate the effectiveness of the RPM program for blood pressure management. The initial inclusion criterion required patients to be on the program for at least 90 days, as this period is necessary to observe adherence to care plans and the effects of data-driven clinical decisions and medication adjustments. This criterion reduced the dataset to 39,988 patients monitored for blood pressure.
Effects on Hypertension Management
Patients were categorized based on engagement levels using the Centers for Medicare & Medicaid Services (CMS) criteria for RPM participation eligibility, which requires approximately 50% participation (16 days in a 30-day period) for related billing.
-
Engaged Patients: Those with a Transmission Index (TI) of 50% or more (22,037 patients, 55.2%) with an average TI of 74.8%.
-
Less-Engaged Patients: Those with a TI of less than 50% (17,951 patients, 44.8%) with an average TI of 24.3%.
Both groups showed significant reductions in systolic blood pressure compared to baseline:
-
Less-Engaged Patients: Experienced an average SBP reduction of 5.8 mmHg, from 138.2 mmHg to 132.4 mmHg.
-
Engaged Patients: Saw a greater reduction of 8.3 mmHg, from 135.5 mmHg to 127.3 mmHg.
Relationship Between RPM Transmission Index (TI%) and Hypertension Management
HealthSnap’s internal data suggests that the frequency of data transmission is positively correlated with improved blood pressure control. Using machine modeling and predictive analytics, it was observed that each 1% increase in the TI is associated with an approximate 0.07 mmHg decrease in SBP.
When patients with initial hypertensive measurements (≥130/80 mmHg) were categorized into quartiles based on their TI%, the results showed significantly greater SBP improvements with higher data transmission frequencies:
-
Quartile 1 (TI 10-24.3%): 6.9 mmHg reduction in SBP.
-
Quartile 2 (TI 24.4-52.3%): 9.8 mmHg reduction in SBP.
-
Quartile 3 (TI 52.4-75.4%): 11.4 mmHg reduction in SBP.
-
Quartile 4 (TI 75.5-100%): 13.7 mmHg reduction in SBP.
Relationship Between RPM Transmission Index (TI%) and Hypertension Management (Control & Stage 1/2)
Among the 22,037 patients who met the inclusion criteria of having a TI of at least 50% and being on the program for a minimum of 90 days, baseline blood pressure measures were compared to the most recent seven data transmissions:
-
Control Range (<130/80 mmHg): 6,952 patients (31.5%) at baseline, increasing to 11,332 patients (51.4%) in the control range by Q2 2024.
-
Stage 1 Hypertension: 6,624 patients (30.1%) at baseline, decreasing slightly to 6,714 patients (30.5%).
-
Stage 2 Hypertension: 8,461 patients (38.4%) at baseline, decreasing to 3,991 patients (18.1%).
For patients with uncontrolled hypertension (SBP ≥130 mmHg or DBP ≥80 mmHg) at baseline:
-
Controlled BP by Q2 2024: 4,472 out of 11,540 patients (38.8%) achieved controlled BP levels.
-
Improvement in SBP: 84.2% showed improved SBP in their recent transmissions.
For patients with Stage 2 hypertension (SBP ≥140 mmHg or DBP ≥90 mmHg) at baseline:
-
Improvement Below Stage 2: 5,726 out of 8,476 patients (67.8%) improved to levels below Stage 2.
-
Improvement in SBP: 88.2% of these patients showed improved SBP in their recent readings.

RPM-Induced Improvements Among Patients with Uncontrolled Hypertension
Patients with baseline hypertension (SBP ≥130 mmHg or DBP ≥80 mmHg) showed significant improvements:
-
Systolic Blood Pressure: Decreased by 14.1 mmHg, from 145.5 mmHg to 131.5 mmHg.
-
Diastolic Blood Pressure: Decreased by 8.0 mmHg, from 84.6 mmHg to 76.6 mmHg.
-
Mean Arterial Pressure: Decreased by 10 mmHg, from 104.9 mmHg to 94.9 mmHg.
RPM-Induced Improvements Among Patients with Systolic and Diastolic Stage 2 Hypertension
Patients with Stage 2 hypertension showed significant improvements:
-
Systolic Blood Pressure: Decreased by 23.8 mmHg.
-
Diastolic Blood Pressure: Decreased by 14.5 mmHg, from 96.8 mmHg to 82.3 mmHg.
-
Mean Arterial Pressure: Decreased by 17.6 mmHg, from 116.9 mmHg to 99.3 mmHg.
Relationship Between RPM Program Duration and Changes in Mean Arterial Pressure
The effects of program duration on blood pressure improvements were analyzed by comparing the most recent data transmissions, with RPM program duration categorized into quartiles:
-
Quartile 1 (90-160 days): MAP decreased by 8.5%.
-
Quartile 2 (161-279 days): MAP decreased by 8.7%.
-
Quartile 3 (280-423 days): MAP decreased by 8.9%.
-
Quartile 4 (424-1,534 days): MAP decreased by 10.6%.
Quartile 4 exhibited significantly greater MAP improvements than all other quartiles, underscoring the importance of longer program duration for better blood pressure management. To learn more, read HealthSnap’s 2024 Clinical Outcomes Report.
Research Study Shows Remote Patient Monitoring Improves Hypertension Management
Hypertension (HTN) is a chronic condition that requires continuous monitoring to manage effectively. Traditional methods like clinic visits and self-reported blood pressure readings often fall short because they don’t provide enough data to track the condition closely. Remote Patient Monitoring offers a solution by allowing continuous monitoring of blood pressure, which can lead to better management of HTN.
Study Details
A research study involving 6,595 patients who were part of a Remote Patient Monitoring program provides evidence that RPM can significantly improve blood pressure control in individuals with hypertension. These patients, who were already receiving traditional treatment, were given blood pressure monitors that sent their readings directly to healthcare providers via cellular networks. The average time participants spent in the RPM program was 289 days.
-
Patient Profile:
-
66.3% of participants had uncontrolled hypertension.
-
37.5% had stage 2 hypertension, a more severe form of the condition.
-
Study Results
After participating in the RPM program for at least 90 days, there were significant improvements:
-
The number of patients with uncontrolled hypertension dropped from 66.3% to 40.2%.
-
Those with stage 2 hypertension saw a reduction from 37.5% to 19.1%.
-
On average, systolic blood pressure (the top number) decreased by 7.3 mmHg across all patients and by 16.7 mmHg for those with stage 2 hypertension.
-
The Mean Arterial Pressure, which is another indicator of overall blood pressure control, improved by 8.5 mmHg in patients with uncontrolled hypertension.
Study Conclusions
This study shows a strong connection between Remote Patient Monitoring and better blood pressure control. When RPM is integrated with electronic health records and supported by regular patient counseling, it can lead to significant health benefits. These include reducing the risk of hypertension-related health issues, such as heart attacks, strokes, and other complications.
-
Long-term Benefits: The study suggests that the benefits of RPM may increase over time, particularly for those who continue the program for a year or more.
-
Data Transmission: Regular data transmission was linked to better blood pressure management, emphasizing the importance of patient engagement in the process.
-
Future Research: The study highlights the need for further research, including controlled trials, to explore the long-term impact of RPM on patient-reported outcomes and healthcare costs.
Economic and Accessibility Benefits of Virtual Care Management Programs
Beyond clinical outcomes, VCM programs offer significant economic and accessibility benefits. By reducing the need for frequent in-person visits and hospitalizations, RPM and CCM programs can lower healthcare costs. Patients also experience fewer out-of-pocket expenses related to emergency care and hospital admissions.

Furthermore, VCM programs enhance healthcare accessibility, particularly for underserved populations. Patients living in remote areas or those with mobility issues can receive consistent care through RPM and CCM, ensuring that they do not fall through the cracks of the healthcare system. This approach levels the playing field, providing all patients with the opportunity to manage their health effectively.
Challenges and Future Directions
While the benefits of VCM programs are clear, challenges remain in their widespread adoption. Ensuring patient engagement and adherence to these programs is critical for their success. With that said, integrating VCM programs with existing healthcare infrastructure, such as Electronic Health Records, requires careful planning and investment.
Future research should focus on refining these programs to maximize their impact on hypertension and other chronic conditions. This includes exploring the long-term benefits of RPM and CCM, the role of patient-reported outcomes, and the potential for cost reductions across healthcare systems.
Choose the Trusted Virtual Care Management Program for Your Healthcare Organization
HealthSnap’s integrated Virtual Care Platform is designed as the ultimate operating system for virtual chronic disease management and unifies your team with near real-time data, personalized patient interactions, and proactive clinical decision-making. Elevate your care delivery with HealthSnap today. Call us at 888-780-1872 or contact us online to schedule a consultation or a demo with our team.






