Evidence-Based Recommendations for a New Standard of Care
Hypertension remains one of the most significant modifiable risk factors for cardiovascular disease, stroke, and mortality. Despite advancements in pharmacologic and lifestyle interventions, a substantial portion of patients remain uncontrolled, contributing to increased morbidity and healthcare costs. Remote Patient Monitoring (RPM) has emerged as a powerful tool for improving hypertension management, enabling continuous blood pressure tracking, real-time clinical insights, and enhanced patient engagement. HealthSnap’s RPM program has demonstrated significant improvements in blood pressure control, adherence patterns, and overall patient outcomes, making it a compelling case for redefining the standard of care in cardiology practices.
This white paper presents evidence-based findings from HealthSnap’s RPM program and outlines key recommendations for implementing RPM as a standard intervention in hypertension management.
Hypertension Status at Baseline and Improvement with RPM
Uncontrolled Hypertension
Among 9,995 cardiology patients with uncontrolled hypertension at baseline (SBP ≥130 mmHg or DBP ≥80 mmHg), 33.7% achieved blood pressure control after RPM intervention. The mean SBP reduction was -9.5 mmHg, and the DBP reduction was -5.7 mmHg. The average duration of the RPM program was 407 ± 313 days, with a transmission index of 64.8%, demonstrating high engagement in BP monitoring. Additionally, 77% of patients showed improvement in Mean Arterial Pressure (MAP), with an average MAP reduction of -6.5% (-7.0 mmHg).
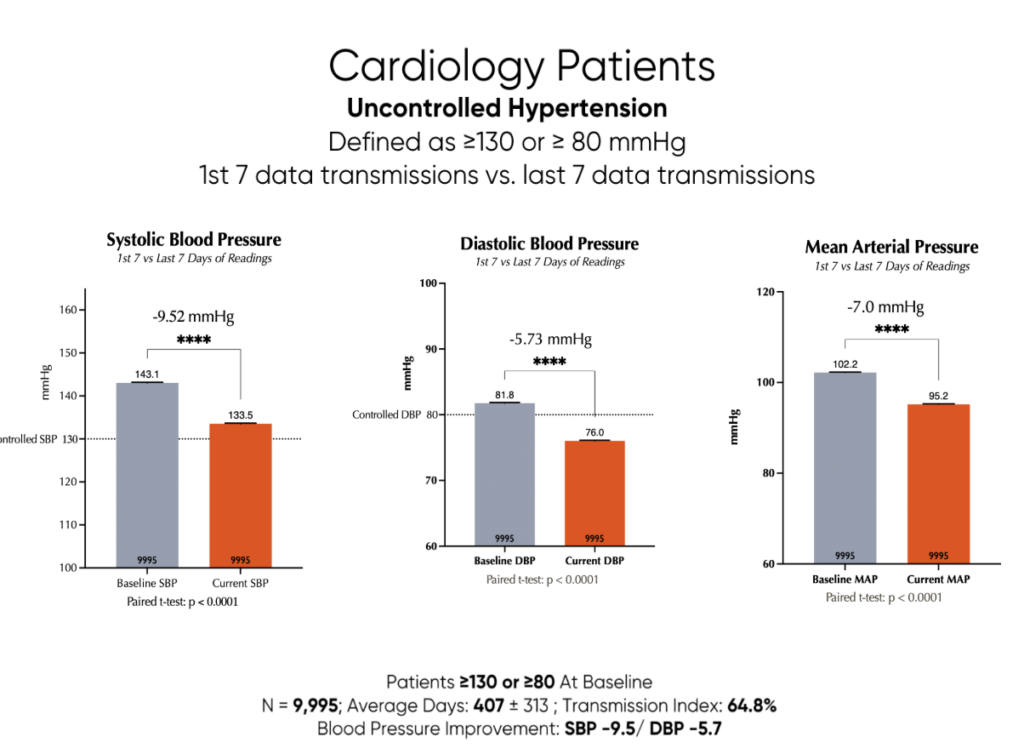
Figure 1: Blood Pressure Improvements Among RPM Patients with Uncontrolled Hypertension
Discussion:
The fact that one-third of patients with uncontrolled hypertension achieved blood pressure control through RPM highlights the potential of this intervention. The reductions in SBP, DBP, and MAP, while modest on average, are clinically significant and can translate to reduced cardiovascular risk over time. The high transmission index suggests that patients are actively participating in the monitoring program, which is crucial for its success. The improvement in MAP further underscores the comprehensive benefits of RPM in managing blood pressure.
Stage 2 Hypertension
Among 5,519 patients with Stage 2 hypertension (SBP ≥140 mmHg or DBP ≥90 mmHg), RPM resulted in significant improvements: 58.9% of patients achieved blood pressure control (SBP <140 mmHg and DBP <90 mmHg) (Figure 2). The mean SBP reduction was -14.5 mmHg, and the DBP reduction was -8.1 mmHg. The average MAP reduction was -9.3%, with 86% of patients showing MAP improvement. Patients remained engaged in the RPM program for an average of 413 ± 315 days, with a transmission index of 63.8%.
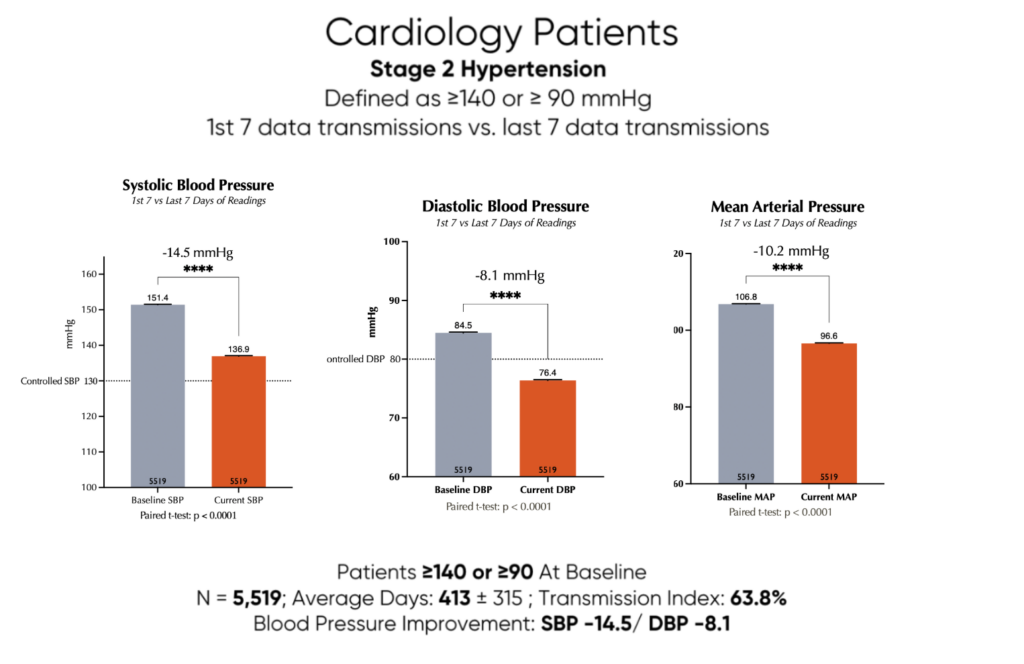
Figure 2: Blood Pressure Improvements Among RPM Patients with Stage 2 Hypertension
Discussion:
The higher percentage of patients achieving blood pressure control in the Stage 2 hypertension group compared to the uncontrolled hypertension group suggests that RPM may be particularly effective for patients with more elevated baseline blood pressures. The greater reductions in SBP, DBP, and MAP further support this notion. The high percentage of patients showing MAP improvement indicates that RPM is having a broad positive impact on blood pressure control in this population.
Severe Hypertension
For 1,374 patients with severe hypertension (SBP ≥140 and DBP ≥90 mmHg), RPM demonstrated remarkable reductions in blood pressure (Figure 3): Mean SBP reduction of -20.7 mmHg and DBP reduction of -13.4 mmHg. MAP reduction of -15.9 mmHg. A high engagement rate, with patients averaging 436 ± 297 days on the program and a transmission index of 61.8%.
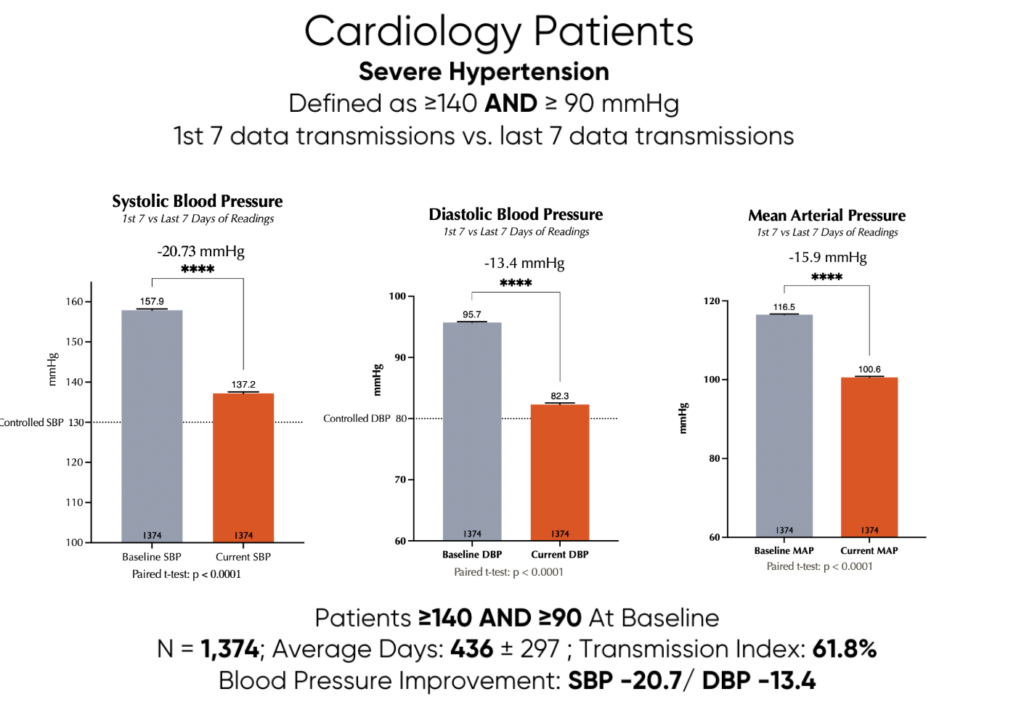
Figure 3: Blood Pressure Improvements Among RPM Patients with Severe Hypertension
Discussion:
The most striking results were observed in the severe hypertension group, with substantial reductions in SBP, DBP, and MAP. These findings suggest that RPM can be a powerful tool for managing even the most challenging cases of hypertension. The high engagement rate in this group is particularly encouraging, as it indicates that patients with severe hypertension are willing to actively participate in their care when provided with the right tools and support. The magnitude of blood pressure reduction in this group is likely to have a significant impact on reducing their risk of cardiovascular events.
Effects of RPM Data Transmission on Blood Pressure Management
Impact of Transmission Frequency
Although ANOVA did not reveal significant differences between groups, each group demonstrated highly significant improvements from baseline: Among 5,093 patients with baseline SBP ≥140 mmHg, blood pressure improvements were analyzed based on RPM data transmission frequency (Figure 4): Patients transmitting 16+ days per 30-day period had the greatest absolute SBP reduction (-16.1 mmHg). Even those transmitting data 5–10 times per 30-day period experienced meaningful reductions (-12.1 mmHg, p < 0.0001 vs. baseline).
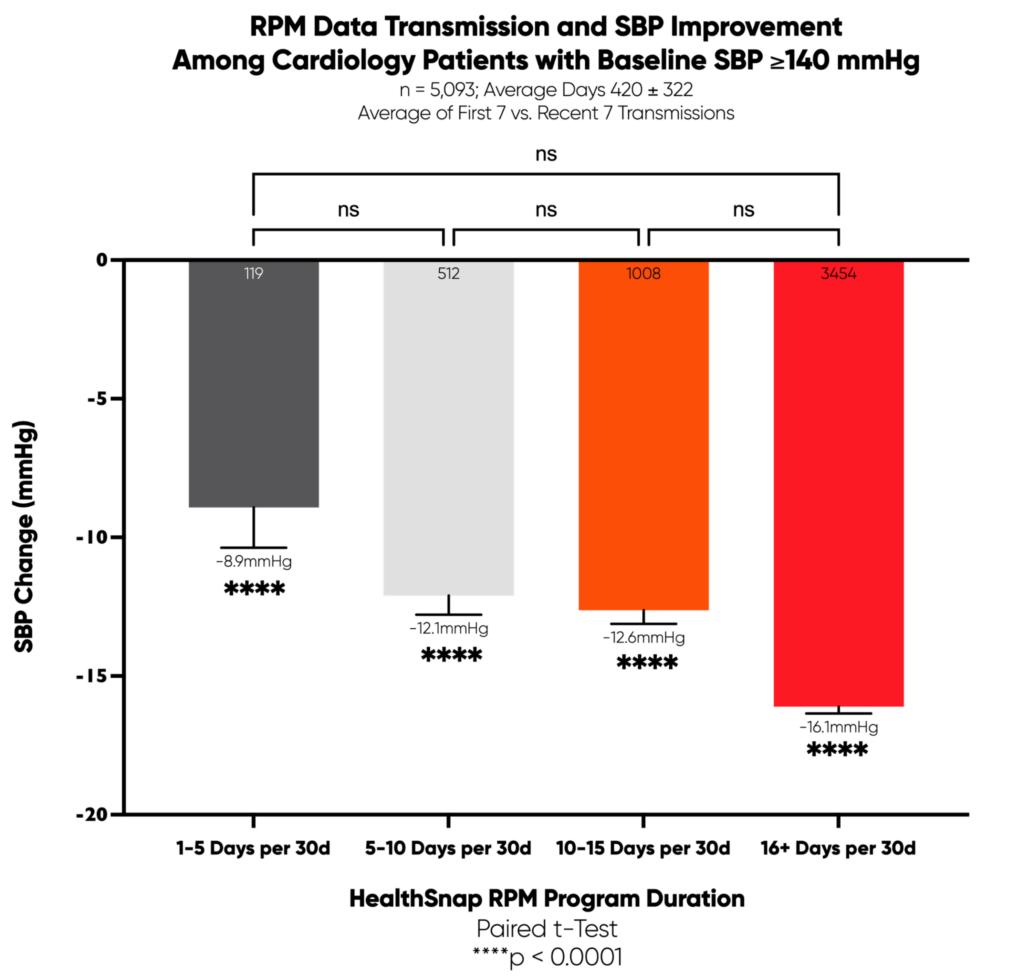
Figure 4: Improvements in SBP among patients w/ SBP ≥140 and Transmission Freq. per 30 days
Discussion:
The finding that more frequent data transmission is associated with greater blood pressure reductions is consistent with the idea that regular monitoring and feedback can help patients stay engaged in their care and make necessary lifestyle adjustments. While the ANOVA results were not significant, the highly significant improvements from baseline in all groups suggest that even infrequent data transmission can be beneficial. This highlights the importance of encouraging patients to transmit their blood pressure data as often as possible, while also recognizing that even occasional monitoring can lead to positive outcomes.
Impact of Transmission Frequency on Clinically Meaningful BP Reduction
A separate analysis examined the percentage of patients achieving a ≥10 mmHg SBP reduction by transmission frequency (Figure 5): 66.2% of patients transmitting 16+ days per 30-days achieved a 10 mmHg reduction. Patients transmitting data 5–10 times per 30-days still saw significant improvements (51.5%, p < 0.0001).
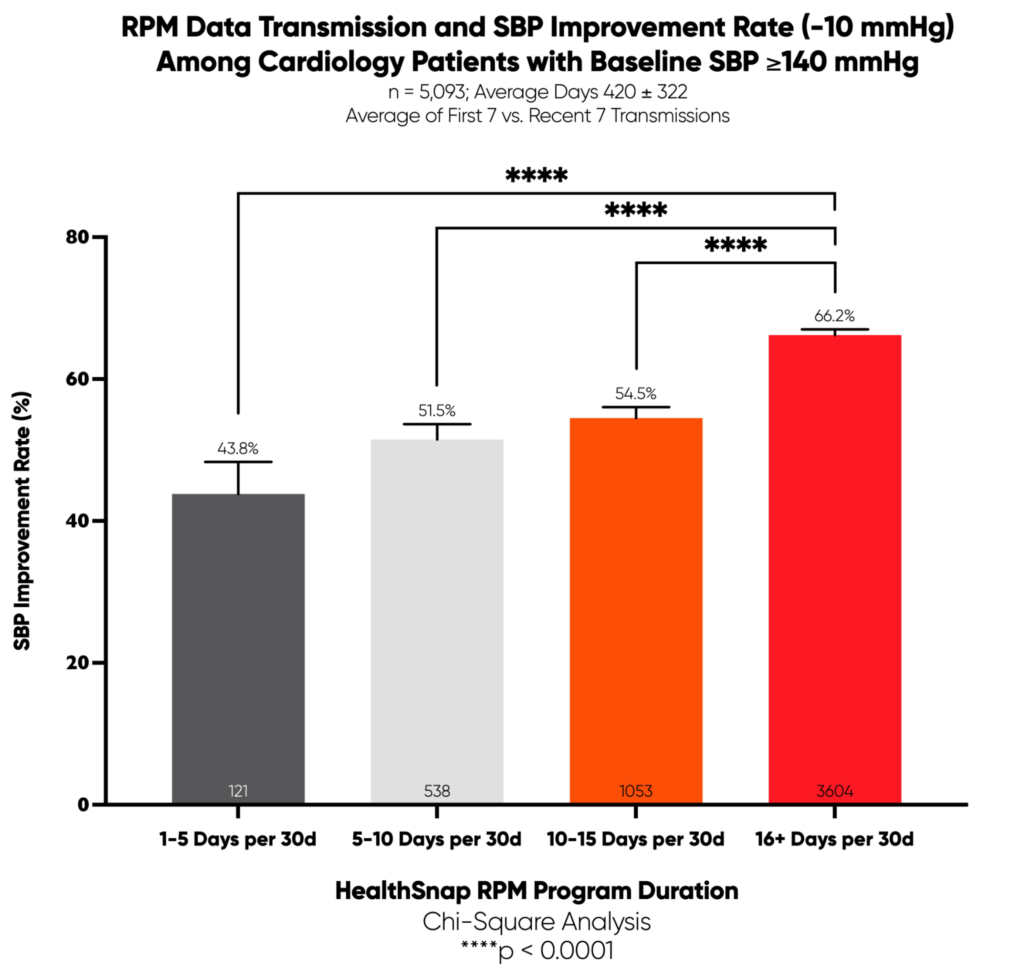
Figure 5: Percentage of Patients Achieving Clinically Meaningful BP Reduction by Transmission Frequency
Discussion:
The fact that a higher percentage of patients achieved a clinically meaningful blood pressure reduction with more frequent data transmission further reinforces the importance of regular monitoring. The 10 mmHg reduction threshold is considered clinically significant because it is associated with a reduced risk of cardiovascular events. The finding that even patients transmitting data 5-10 times per 30 days saw significant improvements suggests that there is a dose-response relationship between transmission frequency and blood pressure control.
Impact of Program Duration
The longitudinal analysis depicted in Figures 6 and 7 underscores the effectiveness of RPM as a long-term intervention and standard of care for hypertension management. Figure 6 highlights a clear trend toward greater improvement in SBP over extended durations of RPM engagement. Patients who remained enrolled for over three years achieved significantly higher improvement rates (73.9%) compared to those monitored for shorter durations (e.g., 55.0% improvement in the 90–210-day cohort). Figure 7 further reinforces this relationship by illustrating progressively greater reductions in SBP with increased duration of RPM participation, highlighting an impressive 19.7 mmHg reduction in patients who remained engaged beyond three years. The statistical analysis was performed using Chi-Square testing, demonstrating significant differences across program duration categories (*p < 0.05, ***p < 0.001, ****p < 0.0001).
Together, these findings strongly advocate for the sustained use of RPM, demonstrating not only immediate clinical benefits but also amplified long-term improvements in patient outcomes. The robust statistical significance and clear incremental benefits observed over time provide compelling evidence to position RPM as an essential component of chronic hypertension management.
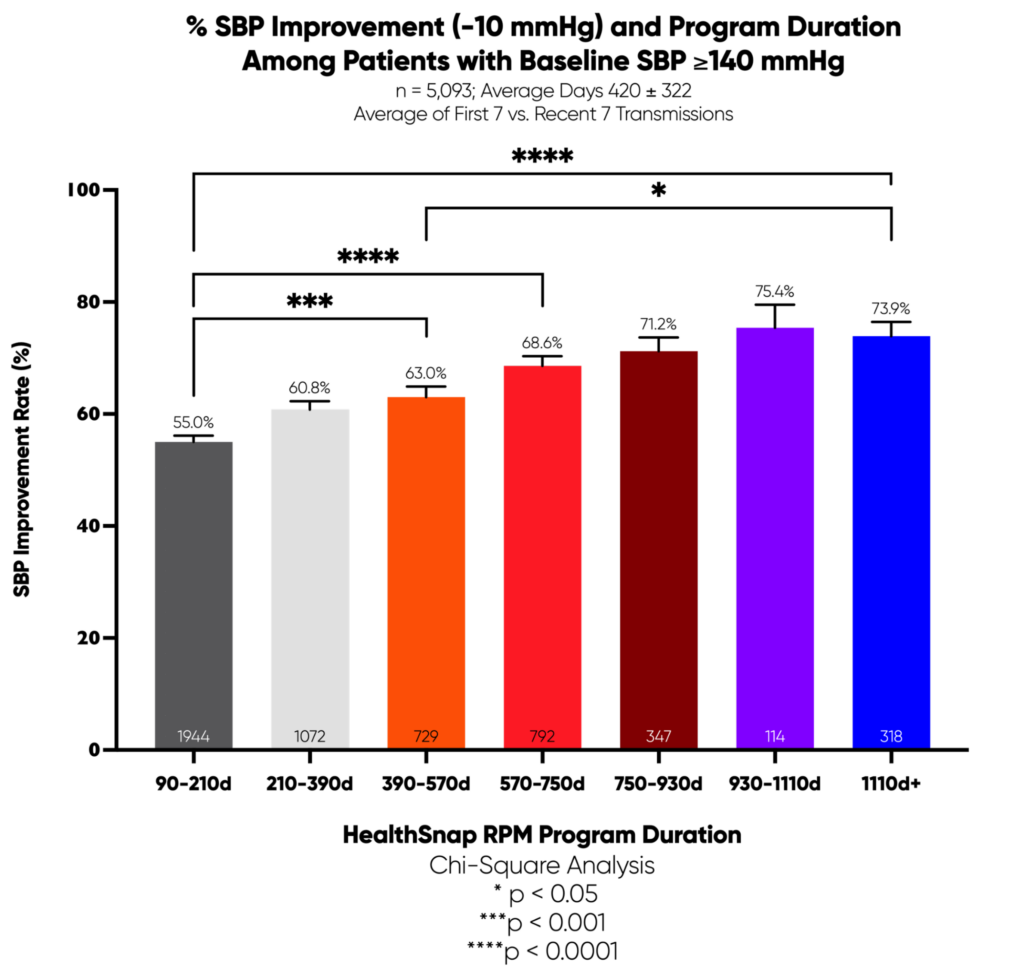
Figure 6: Relationship Between RPM Duration and Rate of 10 mmHg BP Reduction%
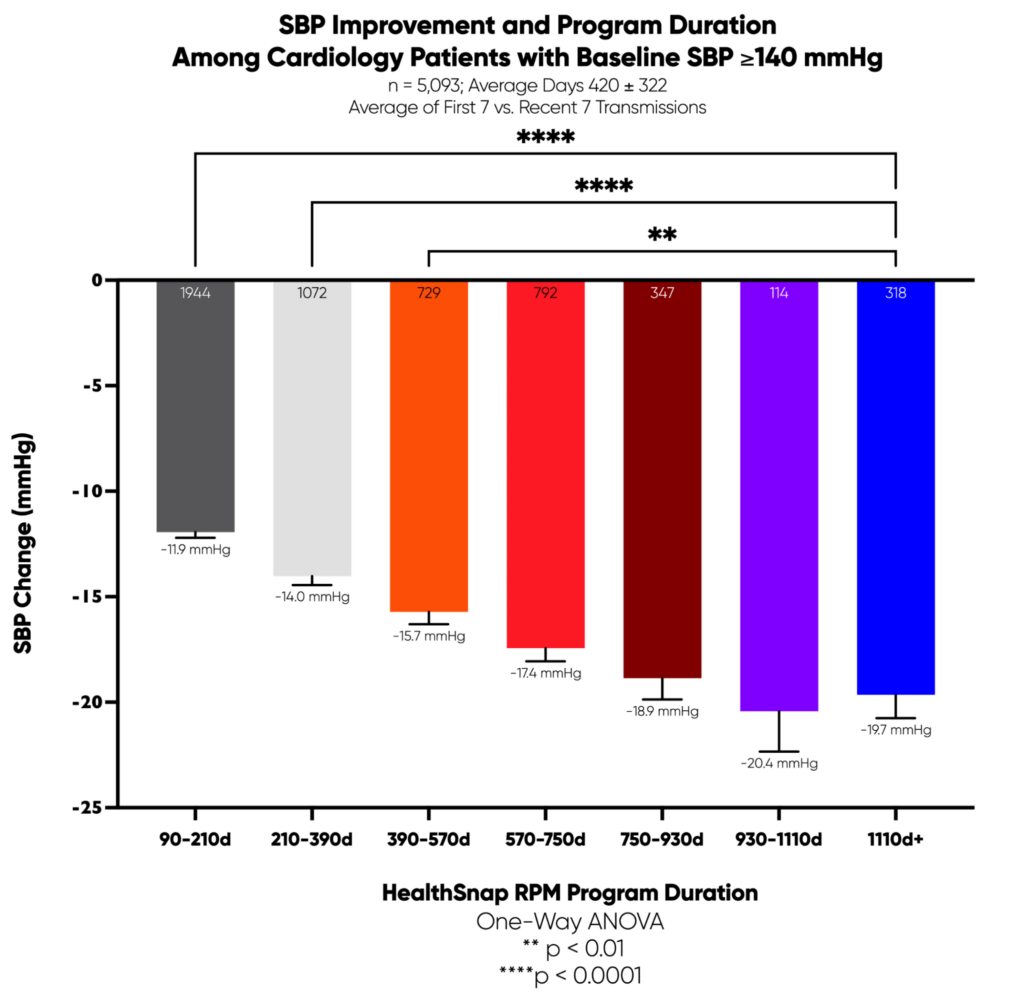
Figure 7: Relationship Between RPM Duration and Reduction in SBP (mmHg)
Discussion:
The positive correlation between program duration and blood pressure reduction is not surprising, as it takes time for patients to make lifestyle changes and for medications to be adjusted to achieve optimal blood pressure control. The fact that patients enrolled for more than one year had the highest success rate suggests that long-term engagement in RPM is necessary to sustain blood pressure control and reduce cardiovascular risk. The significant improvement seen in patients enrolled for 90-180 days indicates that even relatively short-term engagement in RPM can be beneficial.
Impact of RPM Billing Units on Blood Pressure Reduction
An analysis of RPM CPT code utilization (99457/99458) and BP improvements found a direct correlation (Figure 8): Patients receiving 3–6 RPM billing units per year had the highest likelihood (65.4%) of achieving a ≥10 mmHg SBP reduction. Patients with fewer than 3 billing units per year had significantly lower success rates (54.8%).
Notably, many patients who accumulated higher numbers of RPM billing units for telehealth consultations did so due to frequent alerts triggered by rising blood pressure trends or escalation thresholds, such as a hypertensive crisis (SBP ≥180 mmHg or DBP ≥120 mmHg). These alerts prompted clinical interventions, leading to increased patient engagement, more frequent check-ins, and adjustments to treatment plans. The strong correlation between higher transmission frequency and improved blood pressure outcomes reinforces the importance of proactive monitoring and early intervention in hypertension management.
.
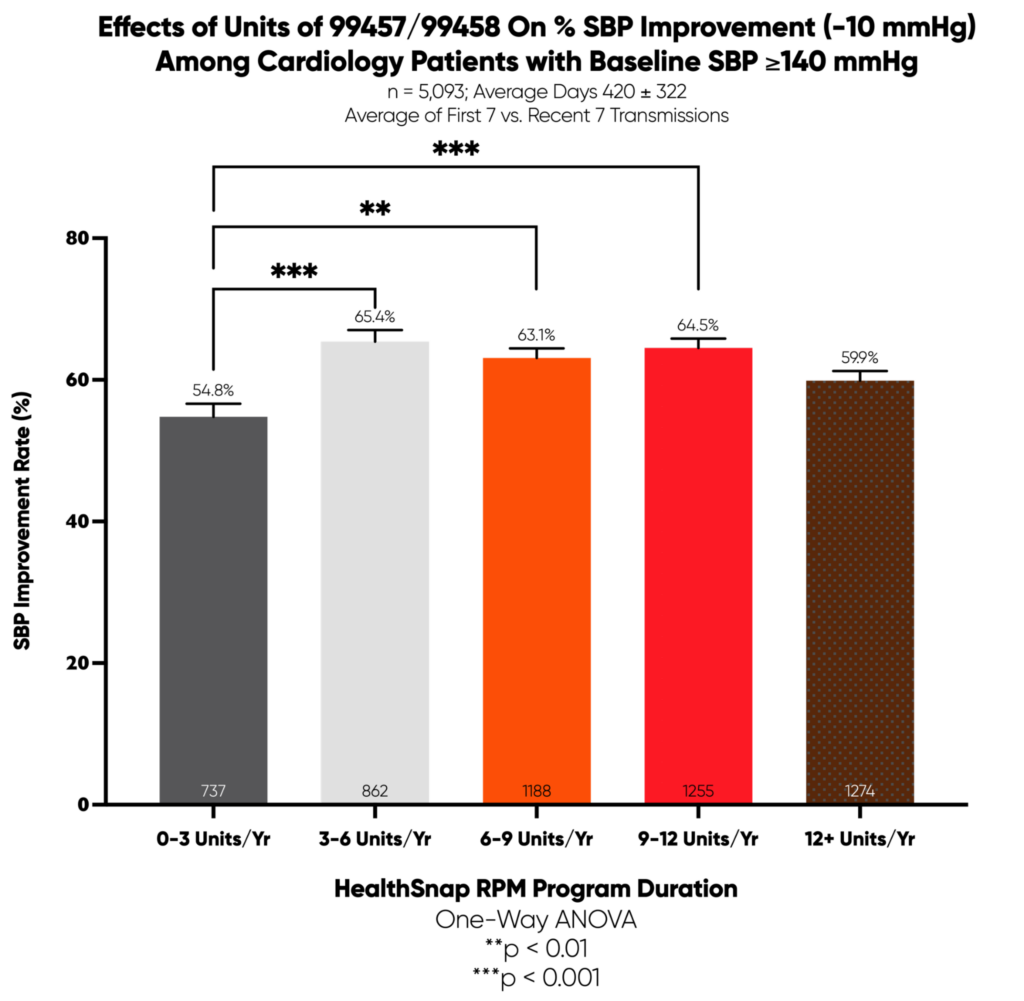
Figure 8: RPM Billing Utilization and BP Reduction
Discussion:
The correlation between RPM billing unit utilization and blood pressure reduction is an interesting finding that warrants further investigation. Patients who receive more RPM billing units may be also receiving more intensive monitoring and support, which leads to better blood pressure control. The fact that many patients with higher billing unit utilization experienced frequent alerts due to rising blood pressure trends suggests that RPM is effectively identifying and addressing blood pressure excursions before they lead to serious complications. This highlights the importance of proactive monitoring and early intervention in hypertension management.
Evidence-Based Recommendations for RPM in Cardiology Practices
Adopt RPM as a Standard of Care
- RPM effectively reduces SBP, DBP, and MAP across all hypertension categories, even among patients treated with medication for a year or longer.
- Provides long-term engagement and continuous BP monitoring.
- Increases accessibility to hypertension management.
Optimize Transmission Frequency
- While 16+ transmissions per 30 days yield the greatest BP reduction, even 5–10 transmissions per 30 days result in meaningful improvement.
Encourage Long-Term Participation
- Patients enrolled for more than one year have the highest likelihood of achieving significant BP reductions.
Conclusion
HealthSnap’s RPM program has demonstrated compelling evidence that remote monitoring is a highly effective intervention for hypertension management in cardiology practices. With significant reductions in blood pressure, high patient engagement, and clear correlations between adherence, transmission frequency, and outcomes, RPM should be considered a new standard of care for hypertension management. By adopting evidence-based RPM practices, cardiology clinics can improve patient outcomes, reduce healthcare costs, and advance hypertension management toward a more proactive and data-driven future.
To learn more about the HealthSnap RPM solution, please book time with our team here.