Chronic diseases, such as diabetes, hypertension, and heart disease, are a growing concern nationwide. To effectively manage these conditions and improve patient outcomes, healthcare providers are increasingly turning to Virtual Care Management programs like Chronic Care Management (CCM). With advancements in technology, virtual care has emerged as a key component of CCM, enabling healthcare providers to remotely monitor and support patients. In this guide, we will explain the steps involved in starting and scaling a CCM Program in 2023.
Understand the CCM Program Requirements
Before launching a CCM program, it is essential to have a comprehensive understanding of the program requirements. The Centers for Medicare and Medicaid Services (CMS) in the United States have specific guidelines for CCM programs, including eligibility criteria, documentation requirements, and billing regulations. Familiarize yourself with these guidelines to ensure compliance and maximize reimbursement opportunities.
Build a Multidisciplinary Care Team
Assemble a multidisciplinary care team to deliver comprehensive care in your CCM program. This team should include qualified healthcare professionals such as physicians, clinical nurse specialists, care coordinators, and any other qualified healthcare specialists relevant to your target population. Ensure that each team member understands their roles and responsibilities within the CCM program.
Identify, Educate, and Enroll Eligible Patients
Finding eligible patients for your Chronic Care Management services program is a key step in ensuring its success. Here are several effective strategies to identify, educate and enroll eligible patients for your CCM program:
Review Electronic Health Records (EHRs)
Start by reviewing your organization’s electronic health records to identify patients with chronic conditions who could benefit from CCM services. Look for patients with conditions such as diabetes, hypertension, heart disease, asthma, or chronic obstructive pulmonary disease (COPD). Analyze their medical history, medication records, and diagnostic codes to determine eligibility.
Collaborate with Health Care Providers and Specialists in Chronic Care Management Services
Engage with primary care providers, specialists, and other healthcare providers within your organization or local healthcare community. Educate them about the benefits of CCM and establish referral pathways for eligible patients.

Implement Risk Stratification Tools
Utilize risk stratification tools to identify high-risk patients who may require intensive care management. These tools use algorithms to analyze patient data and identify individuals with complex or poorly managed chronic conditions. By focusing on high-risk patients, you can optimize your resources and provide targeted interventions.
Leverage Population Health Management Tools
Population health management tools can help identify eligible patients by analyzing and aggregating data from various sources, including claims data, clinical records, and patient-reported information. These tools can help you identify patients with chronic conditions expected who meet the specific criteria for your CCM program and assist in tracking their health status over time.
Engage with Patient Advocacy Groups
Collaborate with patient advocacy groups and community organizations that focus on specific chronic conditions. These groups often have networks of individuals who are actively seeking support and resources to manage their conditions. By establishing partnerships, you can identify eligible patients and raise awareness about your CCM program.
Educate Patients with Chronic Conditions
Implement patient education initiatives to inform individuals about the benefits of CCM and the services offered. Use various channels such as phone calls, emails, brochures, websites, social media, and community events to reach out to patients and their caregivers. Highlight the advantages of CCM, including personalized care, regular check-ins, medication management, and access to a care team.

Utilize Patient Portals and Electronic Communication
Make use of patient portals and electronic communication methods to engage with patients and inform them about your CCM program. Send targeted messages to eligible patients, explaining the program’s benefits and how to enroll. Use the portal to provide educational resources, self-management tools, and appointment reminders.
Train Frontline Staff
Provide training to your frontline staff, including receptionists, nurse practitioners, and medical assistants, to identify and refer eligible patients for the CCM program. These staff members are often the first point of contact for patients, and they can play a vital role in recognizing individuals who may be at significant risk and meet the criteria for enrollment.
Offer Incentives for Enrollment
Consider offering incentives to encourage patients to enroll in your CCM program. This could include benefits such as reduced copayments, access to additional resources or services, or rewards for program adherence and meeting health goals. Ensure that any incentives offered comply with relevant regulations and guidelines.
Remember, it is essential to comply with patient privacy regulations, such as the Health Insurance Portability and Accountability Act (HIPAA), when accessing patient data or communicating with patients. By employing a combination of these strategies, you can effectively identify and enroll eligible patients for your CCM program, ensuring that they receive the comprehensive care and support they need to manage multiple chronic conditions.
Implement Virtual Care Infrastructure
To optimize the benefits of telehealth technologies in your CCM program, you must establish a robust virtual care infrastructure. This includes selecting a secure virtual care platform that facilitates virtual consultations, Remote Patient Monitoring (RPM), and secure communication between patients and care providers. Ensure that the chosen platform complies with privacy regulations, such as HIPAA.
Choose HealthSnap as Your Partner in Success
Choosing the right partner for implementing a Chronic Care Management (CCM) program is crucial to its success. HealthSnap stands out as a reliable and innovative partner for several reasons:
-
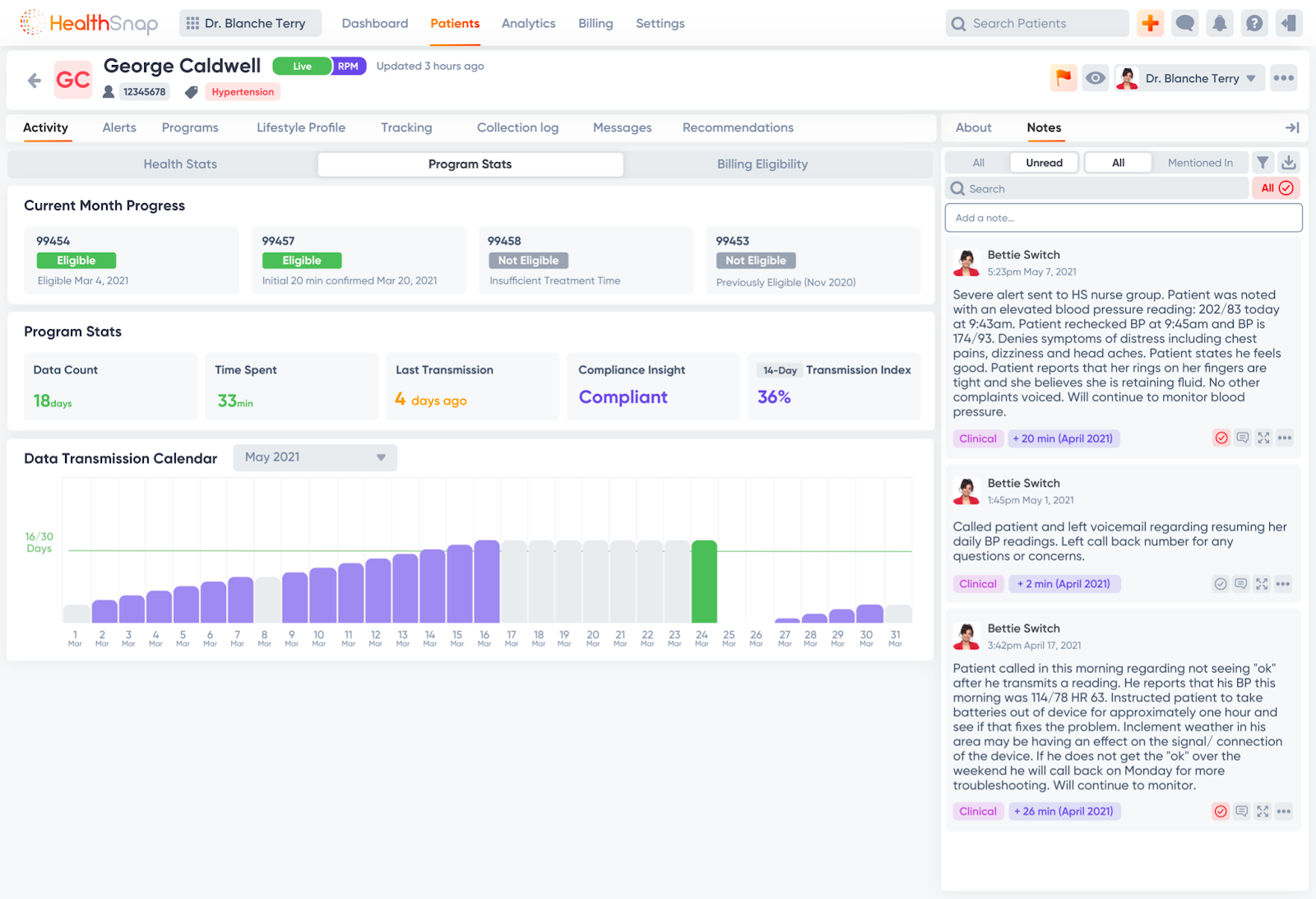
Comprehensive CCM Solution: HealthSnap offers a comprehensive CCM solution that encompasses the key components required for a successful program. HealthSnap’s platform provides features such as Remote Patient Monitoring (RPM), secure communication, care coordination, and data analytics, all integrated into one solution. This allows for seamless implementation and efficient management of the CCM program.
-
Virtual Care Expertise: HealthSnap specializes in virtual care management and understands the importance of leveraging technology to enhance patient care. With HealthSnap’s expertise, healthcare organizations are guided in implementing a CCM program with a strong focus on virtual care, allowing for remote monitoring, video consultations, and secure communication between patients and their care teams.
-
User-Friendly Platform: HealthSnap’s platform is designed with user experience in mind. It is intuitive, easy to navigate, and requires minimal training for both healthcare providers and patients. This user-friendly approach ensures a smooth onboarding process and encourages active patient engagement with the CCM program.
-
Secure and HIPAA-Compliant: HealthSnap prioritizes patient privacy and data security. Our platform is built to comply with the Health Insurance Portability and Accountability Act (HIPAA) regulations, ensuring the confidentiality and integrity of patient information. This commitment to security gives healthcare organizations peace of mind when implementing their CCM program.
-
Customization and Integration: We understand that every healthcare organization has unique requirements and workflows, and offer customization options to tailor the Chronic Care Management program to specific needs, ensuring it aligns with existing processes and preferences. With that said, the HealthSnap platform integrates with electronic health record (EHR) systems and other healthcare technologies, allowing for seamless data sharing and streamlined workflows.
-
Analytics and Reporting: The HealthSnap platform provides robust analytics and reporting capabilities. This allows healthcare organizations to track key performance indicators, measure patient outcomes, and identify areas for improvement within their CCM program. Data-driven insights enable evidence-based decision-making and continuous program optimization.
-
Excellent Customer Support: HealthSnap is known for its responsive and reliable customer support. We provide ongoing assistance, training, and technical support to healthcare organizations implementing a CCM program. This ensures a smooth implementation process and ongoing success in managing the program effectively.
-
Proven Track Record: HealthSnap has a proven track record of successfully implementing CCM programs for various healthcare organizations. Our team’s experience and expertise in the field demonstrate an ability to deliver results and improve patient outcomes through innovative solutions.

Develop Care Plans and Protocols
Developing standardized care plans and protocols is vital to ensure consistent and evidence-based care across the CCM program. Collaborate with your care team to create care plans tailored to different chronic conditions, considering treatment guidelines, patient preferences, and goals of care. Regularly review and update these plans to reflect the latest clinical evidence and patient outcomes.
Train and Educate Care Team Members
Providing comprehensive training and education to the care team is vital for the successful implementation of a CCM program. Conduct training sessions to familiarize team members with the program objectives, virtual care technologies, documentation requirements, and care protocols. Offer ongoing education opportunities to keep the team updated on the latest advancements in chronic disease management and virtual care.

Implement Remote Patient Monitoring
Remote Patient Monitoring (RPM) plays a pivotal role in virtual care-based CCM programs. Select cellular-enabled RPM devices that are easy to use, reliable, and can collect relevant patient data, such as blood pressure, blood glucose levels, and weight. Train patients on using these devices and ensure seamless data transmission to the care team. Establish protocols for monitoring and acting upon the collected data.
Establish Care Coordination Processes
Effective care coordination is vital for the success of a CCM program. Assign dedicated care coordinators responsible for patient outreach, care plan adherence, medication management, appointment scheduling, and coordination with other healthcare providers. Implement communication tools that allow secure and efficient communication between care coordinators, patients, and the care team.
Ensure Continuous Patient Engagement
Maintaining patient engagement is crucial for the long-term success of a CCM program. Utilize various strategies, such as patient portals, mobile applications, and educational materials, to actively engage patients in their care. Regularly communicate with patients through virtual visits, phone calls, and secure messaging to address their concerns, provide education, and reinforce care plan adherence.
Monitor Program Performance and Outcomes
Regularly monitor and evaluate the performance and outcomes of your CCM program. Track key metrics such as patient enrollment, care plan adherence, patient satisfaction, and clinical outcomes. Analyze the data to identify areas for improvement and make necessary adjustments to optimize program effectiveness and efficiency.
Scale the Program and Collaborate with Partners
Once your Chronic Care Management program is established and demonstrates positive outcomes, consider scaling it to reach a larger patient population. Collaborate with other healthcare providers, community organizations, and payers to expand the program’s reach and impact. Explore potential partnerships to share resources, data, and best practices for more comprehensive and coordinated care delivery.
Coding and Billing for Chronic Care Management
Medicare and some private payers provide reimbursement for Chronic Care Management services. Coding and billing for CCM services involve specific codes and documentation requirements to ensure proper reimbursement. Here is an overview of the coding and billing considerations for CCM:
CCM CPT Codes
CPT codes are used to report and bill for Chronic Care Management services. The primary CPT codes for CCM are:
-
CPT 99490
-
CPT 99439
-
CPT 99487
-
CPT 99489
Documentation Requirements
To support proper coding and billing for CCM services, the following documentation is necessary:
-
Comprehensive Care Plan
-
Patient Consent
-
Electronic Health Record (EHR) Documentation
Time-Based Billing
Chronic Care Management services are billed based on the total time spent on care management activities. This includes non-face-to-face activities such as care coordination, medication management, and patient education. The time spent on chronic care management including by clinical staff members should be aggregated to meet the minimum time requirements for each CPT code.
Billing Frequency
CCM services can be billed on a monthly basis. Ensure that the appropriate CPT code is selected based on the level of complexity and time spent on care management activities.
It’s essential to stay updated with the latest coding and billing guidelines from CMS and private payers to ensure accurate reimbursement for CCM services.
HealthSnap: The Premier Virtual Care Platform to Deliver CCM Services
Starting and scaling a CCM program with a focus on virtual care can significantly improve the management of chronic conditions and enhance patient outcomes. HealthSnap’s integrated Virtual Care Management platform enables healthcare organizations to bring care teams together to deliver convenient, affordable, and high-quality chronic care management virtually.
HealthSnap’s HIPAA-compliant and HITRUST-certified virtual CCM and RPM solutions help improve patient outcomes and help boost your revenues at the same time.
To learn more about us or to request a demo, call today at 888-780-1872 (Ext. 3) or click here to schedule a consultation.











Leave A Comment
You must be logged in to post a comment.